Tuesday Poster Session
Category: General Endoscopy
P3421 - Unexpected Finding: Pseudomelanosis Duodeni on Surveillance Endoscopy in a Patient With Hemosiderosis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Sathvik Saineni, MBBS
University of Central Florida College of Medicine
Orlando, FL
Presenting Author(s)
Sathvik Saineni, MBBS, Sesha Sai Kanakamedala, MBBS, Vania Zayat, MD, Richard Henriquez, MD, Amar B Mandalia, MD
University of Central Florida College of Medicine, Orlando, FL
Introduction: Pseudomelanosis duodeni (PD) is an extremely rare, incidental, and benign condition characterized by the deposition of dark pigments in the duodenal mucosa. It is important to recognize and differentiate it from other serious conditions with similar physical findings on endoscopy. Here we report a case of a 58-year-old patient undergoing surveillance endoscopy.
Case Description/Methods: A 58-year-old male with a past medical history of hypertension, diabetes mellitus, coronary artery disease, end-stage renal disease, and cirrhosis was undergoing surveillance endoscopy for esophageal varices. The patient's pertinent outpatient medications include iron carbonyl hydralazine, furosemide, and lisinopril.
A liver biopsy four years ago showed increased iron deposition in perisinusoidal Kupffer cells with grade 4 cirrhosis. The patient has increased ferritin levels ranging from 1500-2900 since 2017, with normal iron, transferrin, and ferritin saturation levels. Testing for mutations in the HFE gene was negative.
Discussion: The usual endoscopic finding of pseudomelanosis duodeni is a black, brown, and grey peppered appearance of the duodenal mucosa. The deposits consist of a mixture of pigments, ferrous sulfide being the most common. The pigment is found in the macrophages of the lamina propria, at the apex of the villi.
The etiology is thought to be associated with local tissue injury, altered iron metabolism, and sulfur-containing medications. The Sulfur present in some diuretics binds to iron from absorption or microhemorrhages and accumulates in the macrophages. Chronic kidney disease contributes to the accumulation due to a decrease in sulfur clearance.
The patient reported receiving oral iron therapy and sulfur-containing drugs such as hydralazine and furosemide. He also had hemosiderosis with high ferritin levels that might have contributed to the iron deposition in the duodenum.
Differentiating between PD, iron pill-induced mucositis, clofazimine related pigmentation, diffuse malignant melanoma, brown bowel syndrome and eosinophilic enteritis is crucial, as the management and prognosis vary significantly.
Endoscopic evaluation and histopathological examination are crucial for the diagnosis of Psudeomelanosis duodeni. Further research is needed to elucidate the underlying mechanisms and establish optimal surveillance strategies for this rare condition.

Disclosures:
Sathvik Saineni, MBBS, Sesha Sai Kanakamedala, MBBS, Vania Zayat, MD, Richard Henriquez, MD, Amar B Mandalia, MD. P3421 - Unexpected Finding: Pseudomelanosis Duodeni on Surveillance Endoscopy in a Patient With Hemosiderosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Central Florida College of Medicine, Orlando, FL
Introduction: Pseudomelanosis duodeni (PD) is an extremely rare, incidental, and benign condition characterized by the deposition of dark pigments in the duodenal mucosa. It is important to recognize and differentiate it from other serious conditions with similar physical findings on endoscopy. Here we report a case of a 58-year-old patient undergoing surveillance endoscopy.
Case Description/Methods: A 58-year-old male with a past medical history of hypertension, diabetes mellitus, coronary artery disease, end-stage renal disease, and cirrhosis was undergoing surveillance endoscopy for esophageal varices. The patient's pertinent outpatient medications include iron carbonyl hydralazine, furosemide, and lisinopril.
A liver biopsy four years ago showed increased iron deposition in perisinusoidal Kupffer cells with grade 4 cirrhosis. The patient has increased ferritin levels ranging from 1500-2900 since 2017, with normal iron, transferrin, and ferritin saturation levels. Testing for mutations in the HFE gene was negative.
Discussion: The usual endoscopic finding of pseudomelanosis duodeni is a black, brown, and grey peppered appearance of the duodenal mucosa. The deposits consist of a mixture of pigments, ferrous sulfide being the most common. The pigment is found in the macrophages of the lamina propria, at the apex of the villi.
The etiology is thought to be associated with local tissue injury, altered iron metabolism, and sulfur-containing medications. The Sulfur present in some diuretics binds to iron from absorption or microhemorrhages and accumulates in the macrophages. Chronic kidney disease contributes to the accumulation due to a decrease in sulfur clearance.
The patient reported receiving oral iron therapy and sulfur-containing drugs such as hydralazine and furosemide. He also had hemosiderosis with high ferritin levels that might have contributed to the iron deposition in the duodenum.
Differentiating between PD, iron pill-induced mucositis, clofazimine related pigmentation, diffuse malignant melanoma, brown bowel syndrome and eosinophilic enteritis is crucial, as the management and prognosis vary significantly.
Endoscopic evaluation and histopathological examination are crucial for the diagnosis of Psudeomelanosis duodeni. Further research is needed to elucidate the underlying mechanisms and establish optimal surveillance strategies for this rare condition.

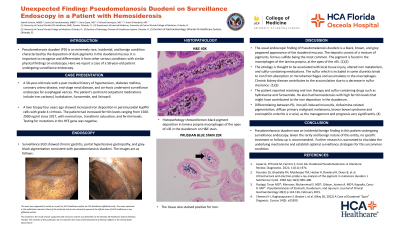
Figure: (A) Surveillance EGD showed chronic gastritis, portal hypertensive gastropathy, and grey-black pigmentation consistent with pseudomelanosis duodeni.
(B) Histopathology showed brown-black pigment deposition in lamina propria macrophages of duodenum on H&E 40x stain.
(C)The tissue stained positive for Iron on Iron Stain 20x.
(B) Histopathology showed brown-black pigment deposition in lamina propria macrophages of duodenum on H&E 40x stain.
(C)The tissue stained positive for Iron on Iron Stain 20x.
Disclosures:
Sathvik Saineni indicated no relevant financial relationships.
Sesha Sai Kanakamedala indicated no relevant financial relationships.
Vania Zayat indicated no relevant financial relationships.
Richard Henriquez indicated no relevant financial relationships.
Amar B Mandalia indicated no relevant financial relationships.
Sathvik Saineni, MBBS, Sesha Sai Kanakamedala, MBBS, Vania Zayat, MD, Richard Henriquez, MD, Amar B Mandalia, MD. P3421 - Unexpected Finding: Pseudomelanosis Duodeni on Surveillance Endoscopy in a Patient With Hemosiderosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
