Tuesday Poster Session
Category: General Endoscopy
P3422 - An Incidental Finding Turned Into a Colonic Polyp Surprise
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Ashwini Mulgaonkar, MD
Scripps Clinic
La Jolla, CA
Presenting Author(s)
Ashwini Mulgaonkar, MD, Liying Fu, MD, Jennifer Au, MD
Scripps Clinic, La Jolla, CA
Introduction: Langerhans cell histiocytosis (LCH) is a relatively rare disease (two to five cases per million per year) that most often is diagnosed in children. Any organ can be involved, and symptoms and severity vary based on location and extent. It ranges from an isolated lesion to systemic involvement. In adults, LCH is often diagnosed incidentally and is less commonly identified than in children.
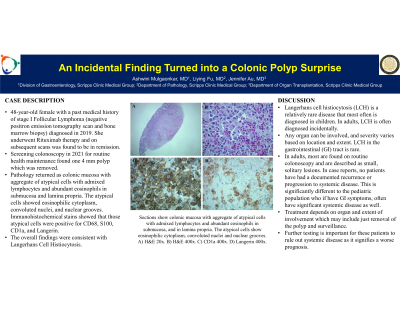
Case Description/Methods: We present a case of a 48-year-old female with a past medical history of stage I Follicular Lymphoma (negative positron emission tomography (PET) scan and bone marrow biopsy) diagnosed in 2019. She underwent Rituximab therapy and on subsequent scans was found to be in remission. She then underwent a screening colonoscopy in 2021 for routine health maintenance. One 4 mm polyp was removed with cold snare and pathology returned as colonic mucosa with aggregate of atypical cells with admixed lymphocytes and abundant eosinophils in submucosa and lamina propria. The atypical cells showed eosinophilic cytoplasm, convoluted nuclei, and nuclear grooves. Immunohistochemical stains showed that those atypical cells were positive for CD68, S100, CD1a, and Langrin. The overall findings were consistent with Langerhans Cell Histiocytosis.
Discussion: LCH in the gastrointestinal (GI) tract is exceedingly rare. Per studies done in the pediatric population, GI involvement portends poor prognosis. It is unclear if that is because in children it is often a part of a greater systemic illness, or due to an isolated risk. In adults, studies of GI involvement are limited to case reports. Most are found on routine colonoscopy and are described as small, solitary lesions. In these case reports, it is interesting that none of the patients had a documented recurrence or progression to systemic disease. This is significantly different to the pediatric population who if present with GI involvement, often have significant systemic disease as well. Unfortunately, there are no standard therapies for adult LCH. Treatment depends on organ and extent of involvement which may include just removal of the polyp, and surveillance.
This is an area that requires continued attention as there are currently no guidelines. Further testing is pertinent for these patients to rule out systemic disease which we do know signifies a worse prognosis compared with isolated lesions. Further studies and evaluation are required to fully understand the importance of LCH in the adult population, especially in the GI tract.

Disclosures:
Ashwini Mulgaonkar, MD, Liying Fu, MD, Jennifer Au, MD. P3422 - An Incidental Finding Turned Into a Colonic Polyp Surprise, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Scripps Clinic, La Jolla, CA
Introduction: Langerhans cell histiocytosis (LCH) is a relatively rare disease (two to five cases per million per year) that most often is diagnosed in children. Any organ can be involved, and symptoms and severity vary based on location and extent. It ranges from an isolated lesion to systemic involvement. In adults, LCH is often diagnosed incidentally and is less commonly identified than in children.
Case Description/Methods: We present a case of a 48-year-old female with a past medical history of stage I Follicular Lymphoma (negative positron emission tomography (PET) scan and bone marrow biopsy) diagnosed in 2019. She underwent Rituximab therapy and on subsequent scans was found to be in remission. She then underwent a screening colonoscopy in 2021 for routine health maintenance. One 4 mm polyp was removed with cold snare and pathology returned as colonic mucosa with aggregate of atypical cells with admixed lymphocytes and abundant eosinophils in submucosa and lamina propria. The atypical cells showed eosinophilic cytoplasm, convoluted nuclei, and nuclear grooves. Immunohistochemical stains showed that those atypical cells were positive for CD68, S100, CD1a, and Langrin. The overall findings were consistent with Langerhans Cell Histiocytosis.
Discussion: LCH in the gastrointestinal (GI) tract is exceedingly rare. Per studies done in the pediatric population, GI involvement portends poor prognosis. It is unclear if that is because in children it is often a part of a greater systemic illness, or due to an isolated risk. In adults, studies of GI involvement are limited to case reports. Most are found on routine colonoscopy and are described as small, solitary lesions. In these case reports, it is interesting that none of the patients had a documented recurrence or progression to systemic disease. This is significantly different to the pediatric population who if present with GI involvement, often have significant systemic disease as well. Unfortunately, there are no standard therapies for adult LCH. Treatment depends on organ and extent of involvement which may include just removal of the polyp, and surveillance.
This is an area that requires continued attention as there are currently no guidelines. Further testing is pertinent for these patients to rule out systemic disease which we do know signifies a worse prognosis compared with isolated lesions. Further studies and evaluation are required to fully understand the importance of LCH in the adult population, especially in the GI tract.

Figure: Colonic mucosa with aggregate of atypical cells with admixed lymphocytes and abundant eosinophils in submucosa and lamina propria. The atypical cells show eosinophilic cytoplasm, convoluted nuclei, and nuclear grooves.
Disclosures:
Ashwini Mulgaonkar indicated no relevant financial relationships.
Liying Fu indicated no relevant financial relationships.
Jennifer Au: Genentech – Consultant.
Ashwini Mulgaonkar, MD, Liying Fu, MD, Jennifer Au, MD. P3422 - An Incidental Finding Turned Into a Colonic Polyp Surprise, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

