Tuesday Poster Session
Category: General Endoscopy
P3437 - Advanced Mantle Cell Lymphoma on Screening Colonoscopy
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Katherine M. Cooper, MD
UMass Chan Medical School
Worcester, MA
Presenting Author(s)
Katherine M.. Cooper, MD, Nicholas Koen, MD, Julia Jennings, MD, Navine Nasser-Ghodsi, MD
UMass Chan Medical School, Worcester, MA
Introduction: Mantle cell lymphoma (MCL) is a B cell lymphoma that originates in the mantle zone of lymph nodes. Extra-nodal (EN) disease is present in 5-20% of cases, but primary EN disease (e.g., gastrointestinal MCL) is rare. We herein present an atypical case of MCL with mixed features identified on screening colonoscopy.
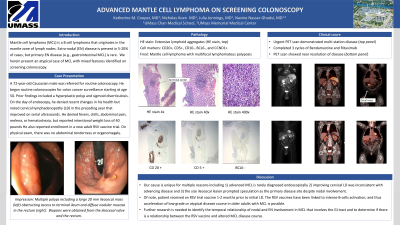
Case Description/Methods: A 72-year-old Caucasian male was referred for routine colonoscopy. He began routine colonoscopies for colon cancer surveillance starting at age 50. Prior findings included a hyperplastic polyp and sigmoid diverticulosis. On the day of endoscopy, he denied recent changes in his health but noted cervical LD in the preceding year that improved on serial ultrasounds. He denied fevers, chills, abdominal pain, melena, or hematochezia, but reported intentional weight loss of 40 pounds with lifestyle modifications. He also reported enrollment in a new adult RSV vaccine trial. On physical exam, there was no abdominal tenderness or organomegaly. Colonoscopy identified multiple polyps including a large 20 mm ileocecal polyp obstructing access to terminal ileum (top left) and diffuse nodular mucosa in the rectum. Biopsies obtained from the ileocecal valve, rectum and ileum showed extensive lymphoid aggregates that were CD20+, CD5+, CD10-, BCL6-, and CCND1+ (left panels), consistent with multifocal lymphomatous polyposis 20 to MCL. Oncology referral was placed and urgent PET scan revealed multi-station LAD consistent with stage IV disease (top panels). The patient completed 3 cycles of Bendamustine and Rituximab; repeat PET scan showed near resolution of disease at all sites (bottom).
Discussion: We present an atypical case of MCL affecting the colon. This case is atypical for multiple reasons: 1) while GI involvement is not uncommon, advanced MCL is rarely diagnosed endoscopically 2) improving cervical LD was inconsistent with advancing disease and 3) the size ileocecal lesion prompted speculation as the primary disease site despite nodal involvement. Interestingly, the patient received an RSV trial vaccine 1-2 months prior to initial LD. The RSV vaccines have been linked to intense B-cells activation, and thus acceleration of low-grade or atypical disease course in older adults with MCL is possible. Further research is needed to identify the temporal relationship of nodal and EN involvement in MCL that involves the GI tract and to determine if there is a relationship between the RSV vaccine and altered MCL disease course.

Disclosures:
Katherine M.. Cooper, MD, Nicholas Koen, MD, Julia Jennings, MD, Navine Nasser-Ghodsi, MD. P3437 - Advanced Mantle Cell Lymphoma on Screening Colonoscopy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
UMass Chan Medical School, Worcester, MA
Introduction: Mantle cell lymphoma (MCL) is a B cell lymphoma that originates in the mantle zone of lymph nodes. Extra-nodal (EN) disease is present in 5-20% of cases, but primary EN disease (e.g., gastrointestinal MCL) is rare. We herein present an atypical case of MCL with mixed features identified on screening colonoscopy.
Case Description/Methods: A 72-year-old Caucasian male was referred for routine colonoscopy. He began routine colonoscopies for colon cancer surveillance starting at age 50. Prior findings included a hyperplastic polyp and sigmoid diverticulosis. On the day of endoscopy, he denied recent changes in his health but noted cervical LD in the preceding year that improved on serial ultrasounds. He denied fevers, chills, abdominal pain, melena, or hematochezia, but reported intentional weight loss of 40 pounds with lifestyle modifications. He also reported enrollment in a new adult RSV vaccine trial. On physical exam, there was no abdominal tenderness or organomegaly. Colonoscopy identified multiple polyps including a large 20 mm ileocecal polyp obstructing access to terminal ileum (top left) and diffuse nodular mucosa in the rectum. Biopsies obtained from the ileocecal valve, rectum and ileum showed extensive lymphoid aggregates that were CD20+, CD5+, CD10-, BCL6-, and CCND1+ (left panels), consistent with multifocal lymphomatous polyposis 20 to MCL. Oncology referral was placed and urgent PET scan revealed multi-station LAD consistent with stage IV disease (top panels). The patient completed 3 cycles of Bendamustine and Rituximab; repeat PET scan showed near resolution of disease at all sites (bottom).
Discussion: We present an atypical case of MCL affecting the colon. This case is atypical for multiple reasons: 1) while GI involvement is not uncommon, advanced MCL is rarely diagnosed endoscopically 2) improving cervical LD was inconsistent with advancing disease and 3) the size ileocecal lesion prompted speculation as the primary disease site despite nodal involvement. Interestingly, the patient received an RSV trial vaccine 1-2 months prior to initial LD. The RSV vaccines have been linked to intense B-cells activation, and thus acceleration of low-grade or atypical disease course in older adults with MCL is possible. Further research is needed to identify the temporal relationship of nodal and EN involvement in MCL that involves the GI tract and to determine if there is a relationship between the RSV vaccine and altered MCL disease course.

Figure: Evaluation of ileocecal mass. Top left panel: endoscopic image of 20 mm ileocecal polypoid mass. Middle left panel: Biopsy tissue evaluation with Hematoxylin and eosin stain. Bottom left: CD 20 staining of the germinal center. Right top = pre-treatment PET scan with FDG uptake tin the spleen and at the area of the cecal valve. Bottom right = Interval PET scan after 3 cycles of Bendamustine and Rituximab showing complete resolution of uptake in both locations.
Disclosures:
Katherine Cooper indicated no relevant financial relationships.
Nicholas Koen indicated no relevant financial relationships.
Julia Jennings indicated no relevant financial relationships.
Navine Nasser-Ghodsi indicated no relevant financial relationships.
Katherine M.. Cooper, MD, Nicholas Koen, MD, Julia Jennings, MD, Navine Nasser-Ghodsi, MD. P3437 - Advanced Mantle Cell Lymphoma on Screening Colonoscopy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
