Tuesday Poster Session
Category: General Endoscopy
P3438 - Double Diaphragmatic Trouble: Concurrent NSAID-Induced Diaphragmatic Strictures in the Small and Large Bowel
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- CI
Christian J. Ie, MD, MS
Madigan Army Medical Center
Joint Base Lewis-McChord, WA
Presenting Author(s)
Christian J. Ie, MD, MS
Madigan Army Medical Center, Joint Base Lewis-McChord, WA
Introduction: Diaphragm disease is a rare complication of non-steroidal anti-inflammatory drug (NSAID) use characterized by the formation of diaphragm-like luminal strictures within the small and/or large bowel. Given the ubiquitous use of NSAIDs for their anti-inflammatory and analgesic properties, provider awareness of this condition and its potential sequelae is crucial for early diagnosis and conducting appropriate interventions.
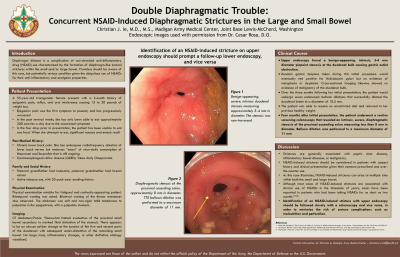
Case Description/Methods: A 55-year-old transgender female with a history of NSAID use for chronic lower back pain presented with a three-month history of prandial epigastric pain, 7–9-kilogram weight loss, acid reflux, and oral intolerance. Upper endoscopy found a benign-appearing, intrinsic, 3-4 mm diameter pinpoint stenosis at the duodenal bulb. Random gastric biopsies taken during this initial procedure would eventually test positive for Helicobacter pylori but found no evidence of metaplasia or dysplasia. Cross-sectional imaging likewise showed no evidence of malignancy of the duodenal bulb. Over the following three months, the patient underwent seven endoscopic balloon dilations that successfully dilated the duodenal lumen to a diameter of 10.5 mm, which resolved her oral intolerance, and reversed her weight loss. The patient discontinued NSAIDs and completed quadruple therapy that successfully eradicated H. pylori. One month after the last endoscopic dilation, the patient underwent a routine screening colonoscopy. This colonoscopy revealed an intrinsic, severe, diaphragmatic stenosis of the proximal ascending colon measuring less than 8 mm in diameter. Balloon dilation was performed to a maximum diameter of 11 mm. Biopsies obtained during this colonoscopy were ultimately negative for features of chronicity, activity, granulomas, or dysplasia.
Discussion: This case provides an example of a debilitating complication of NSAID use and illustrates how NSAID-induced diaphragmatic strictures can concurrently arise at multiple sites in both the small and large bowel. While strictures are generally more associated with peptic ulcer disease, the inflammatory bowel diseases, or malignancy, NSAID-induced strictures should be considered in the differential diagnoses for these strictures given their common prescribed and over-the-counter use. Identification of a stricture with upper endoscopy should be followed closely with a colonoscopy and vice versa, in order to minimize the risk of further complications such as malnutrition and perforation.
The views expressed above are those of the authors and do not reflect the official policy of the Army, Department of Defense, or US Government.

Disclosures:
Christian J. Ie, MD, MS. P3438 - Double Diaphragmatic Trouble: Concurrent NSAID-Induced Diaphragmatic Strictures in the Small and Large Bowel, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Madigan Army Medical Center, Joint Base Lewis-McChord, WA
Introduction: Diaphragm disease is a rare complication of non-steroidal anti-inflammatory drug (NSAID) use characterized by the formation of diaphragm-like luminal strictures within the small and/or large bowel. Given the ubiquitous use of NSAIDs for their anti-inflammatory and analgesic properties, provider awareness of this condition and its potential sequelae is crucial for early diagnosis and conducting appropriate interventions.
Case Description/Methods: A 55-year-old transgender female with a history of NSAID use for chronic lower back pain presented with a three-month history of prandial epigastric pain, 7–9-kilogram weight loss, acid reflux, and oral intolerance. Upper endoscopy found a benign-appearing, intrinsic, 3-4 mm diameter pinpoint stenosis at the duodenal bulb. Random gastric biopsies taken during this initial procedure would eventually test positive for Helicobacter pylori but found no evidence of metaplasia or dysplasia. Cross-sectional imaging likewise showed no evidence of malignancy of the duodenal bulb. Over the following three months, the patient underwent seven endoscopic balloon dilations that successfully dilated the duodenal lumen to a diameter of 10.5 mm, which resolved her oral intolerance, and reversed her weight loss. The patient discontinued NSAIDs and completed quadruple therapy that successfully eradicated H. pylori. One month after the last endoscopic dilation, the patient underwent a routine screening colonoscopy. This colonoscopy revealed an intrinsic, severe, diaphragmatic stenosis of the proximal ascending colon measuring less than 8 mm in diameter. Balloon dilation was performed to a maximum diameter of 11 mm. Biopsies obtained during this colonoscopy were ultimately negative for features of chronicity, activity, granulomas, or dysplasia.
Discussion: This case provides an example of a debilitating complication of NSAID use and illustrates how NSAID-induced diaphragmatic strictures can concurrently arise at multiple sites in both the small and large bowel. While strictures are generally more associated with peptic ulcer disease, the inflammatory bowel diseases, or malignancy, NSAID-induced strictures should be considered in the differential diagnoses for these strictures given their common prescribed and over-the-counter use. Identification of a stricture with upper endoscopy should be followed closely with a colonoscopy and vice versa, in order to minimize the risk of further complications such as malnutrition and perforation.
The views expressed above are those of the authors and do not reflect the official policy of the Army, Department of Defense, or US Government.

Figure: Left: Duodenal bulb stenosis measuring 3-4 mm in diameter
Right: Proximal ascending colon stenosis measuring <9 mm in diameter
Right: Proximal ascending colon stenosis measuring <9 mm in diameter
Disclosures:
Christian Ie indicated no relevant financial relationships.
Christian J. Ie, MD, MS. P3438 - Double Diaphragmatic Trouble: Concurrent NSAID-Induced Diaphragmatic Strictures in the Small and Large Bowel, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
