Tuesday Poster Session
Category: GI Bleeding
P3448 - Risk and Predictors of Hematochezia in Patients With Stool Management Device: A Single Center Retrospective Cohort Study
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Balakrishna Ravella, MBBS, MD
OSF Health St. Mary's Medical Center
Galesburg, IL
Presenting Author(s)
Parth Patel, MD1, Balakrishna Ravella, MBBS, MD2, Suha Abushamma, MD3, Siri Ancha, MD1, Osama Altayar, MD1
1Washington University School of Medicine, St. Louis, MO; 2OSF Health St. Mary's Medical Center, Galesburg, IL; 3Cleveland Clinic, Cleveland, OH
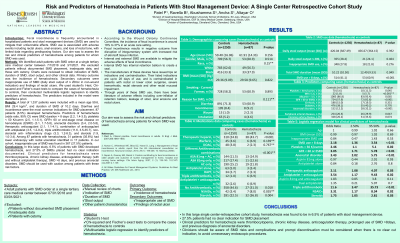
Introduction: Fecal incontinence is frequently encountered in hospitalized patients and stool management devices (SMD) are used to mitigate their unfavorable effects. SMD use is associated with adverse events including rectal ulcers, anal erosions, and loss of rectal tone, with limited data regarding predisposing risk factors. Our aim was to assess the risk and clinical predictors of hematochezia among patients for whom SMD was used.
Methods: We identified adult patients with SMD order at a single tertiary care medical center between 7/1/2018 and 3/1/2021. We excluded patients without documented SMD placement, inadequate data, and those with ostomy. Charts were reviewed to obtain indication of SMD, duration of SMD, stool output, and other clinical data. Primary outcome was the incidence of hematochezia. Secondary outcomes were inappropriate use of SMD (daily stool output of ≤ 200cc in non-wound indication) and findings of rectal ulcers. We used student's t-test, Chi-squared and Fisher’s exact tests to compare the cases of hematochezia to controls, then conducted multivariable logistic regression to identify predictors of hematochezia. The predictors included in the model were identified a priori.
Results: A total of 1,337 patients were included with a mean age 59.6, BMI 29.4 kg/m2, and duration of SMD of 10.2 days. Diarrhea and incontinence were the most common indications for SMD placement. 87 patients (6.5%) developed hematochezia. Predictors of hematochezia (odds ratio, 95% CI) were SMD duration > 8 days (2.2, 1.4-3.5), platelets < 50 K/cumm (2.5, 1.1-5.1), GFR< 60 or end-stage renal disease on hemodialysis (ESRD) (3.1, 1.7-5.8), anorectal disorders (3.4, 2.0-5.8), therapeutic anticoagulant (2.1, 1.1-4.1), combination of anticoagulant with antiplatelet (3.5, 1.2-9.4), triple antithrombotic (11.6, 3.5-35.7), non-steroidal anti-inflammatory drugs (3.3, 1.2-8.3), and steroids (1.9, 1.0-3.4). Among 87 patients with hematochezia, 31 patients (35.6%) had lower endoscopy with rectal ulceration identified in 17 patients. In our cohort, inappropriate use of SMD was found in 367 (27.5%) patients.
Discussion: In this large study, 6.5% of patients with SMD developed hematochezia, and 27.5% of SMDs placed had no clear indication documented. Clinical predictors for hematochezia were thrombocytopenia, chronic kidney disease, anticoagulation therapy (with and without antiplatelet therapy), SMD >8 days, and previous anorectal disorders. SMD should be used with caution among patients with these risk factors.
Disclosures:
Parth Patel, MD1, Balakrishna Ravella, MBBS, MD2, Suha Abushamma, MD3, Siri Ancha, MD1, Osama Altayar, MD1. P3448 - Risk and Predictors of Hematochezia in Patients With Stool Management Device: A Single Center Retrospective Cohort Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Washington University School of Medicine, St. Louis, MO; 2OSF Health St. Mary's Medical Center, Galesburg, IL; 3Cleveland Clinic, Cleveland, OH
Introduction: Fecal incontinence is frequently encountered in hospitalized patients and stool management devices (SMD) are used to mitigate their unfavorable effects. SMD use is associated with adverse events including rectal ulcers, anal erosions, and loss of rectal tone, with limited data regarding predisposing risk factors. Our aim was to assess the risk and clinical predictors of hematochezia among patients for whom SMD was used.
Methods: We identified adult patients with SMD order at a single tertiary care medical center between 7/1/2018 and 3/1/2021. We excluded patients without documented SMD placement, inadequate data, and those with ostomy. Charts were reviewed to obtain indication of SMD, duration of SMD, stool output, and other clinical data. Primary outcome was the incidence of hematochezia. Secondary outcomes were inappropriate use of SMD (daily stool output of ≤ 200cc in non-wound indication) and findings of rectal ulcers. We used student's t-test, Chi-squared and Fisher’s exact tests to compare the cases of hematochezia to controls, then conducted multivariable logistic regression to identify predictors of hematochezia. The predictors included in the model were identified a priori.
Results: A total of 1,337 patients were included with a mean age 59.6, BMI 29.4 kg/m2, and duration of SMD of 10.2 days. Diarrhea and incontinence were the most common indications for SMD placement. 87 patients (6.5%) developed hematochezia. Predictors of hematochezia (odds ratio, 95% CI) were SMD duration > 8 days (2.2, 1.4-3.5), platelets < 50 K/cumm (2.5, 1.1-5.1), GFR< 60 or end-stage renal disease on hemodialysis (ESRD) (3.1, 1.7-5.8), anorectal disorders (3.4, 2.0-5.8), therapeutic anticoagulant (2.1, 1.1-4.1), combination of anticoagulant with antiplatelet (3.5, 1.2-9.4), triple antithrombotic (11.6, 3.5-35.7), non-steroidal anti-inflammatory drugs (3.3, 1.2-8.3), and steroids (1.9, 1.0-3.4). Among 87 patients with hematochezia, 31 patients (35.6%) had lower endoscopy with rectal ulceration identified in 17 patients. In our cohort, inappropriate use of SMD was found in 367 (27.5%) patients.
Discussion: In this large study, 6.5% of patients with SMD developed hematochezia, and 27.5% of SMDs placed had no clear indication documented. Clinical predictors for hematochezia were thrombocytopenia, chronic kidney disease, anticoagulation therapy (with and without antiplatelet therapy), SMD >8 days, and previous anorectal disorders. SMD should be used with caution among patients with these risk factors.
Disclosures:
Parth Patel indicated no relevant financial relationships.
Balakrishna Ravella indicated no relevant financial relationships.
Suha Abushamma indicated no relevant financial relationships.
Siri Ancha indicated no relevant financial relationships.
Osama Altayar indicated no relevant financial relationships.
Parth Patel, MD1, Balakrishna Ravella, MBBS, MD2, Suha Abushamma, MD3, Siri Ancha, MD1, Osama Altayar, MD1. P3448 - Risk and Predictors of Hematochezia in Patients With Stool Management Device: A Single Center Retrospective Cohort Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
