Tuesday Poster Session
Category: GI Bleeding
P3449 - Predictors of Short and Long Term Rebleeding in Patients with Overt Gastrointestinal Bleeding: A Prospective Study
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Kassem Barada, MD
American University of Beirut
Beirut, Beyrouth, Lebanon
Presenting Author(s)
Chantal Rizk, MD1, Anthony Kerbage, MD2, Hani Tamim, PhD1, Walaa G. El Sheikh, BA1, Don C. Rockey, MD3, Kassem Barada, MD1
1American University of Beirut, Beirut, Beyrouth, Lebanon; 2Cleveland Clinic, Cleveland, OH; 3Medical University of South Carolina, Charleston, SC
Introduction: Rebleeding is common in patients with gastrointestinal bleeding (GIB) and is associated with increased morbidity and cost. We examined predictors of rebleeding in patients with overt GIB.
Methods: This was a prospective study of patients admitted to a tertiary care center with acute overt GIB between 2013 and 2023. Patients were followed-up in-hospital and after discharge at 1 month, 1 year and yearly thereafter. Rebleeding was defined by the presence of visualized hematemesis, melena, and/or hematochezia ≥ 24 hours after initial endoscopic evaluation and/or hemostasis and initial stabilization, accompanied by change of vital signs or ≥2 g/dL drop in hemoglobin (Hb). Independent predictors of rebleeding were determined after controlling for relevant confounders.
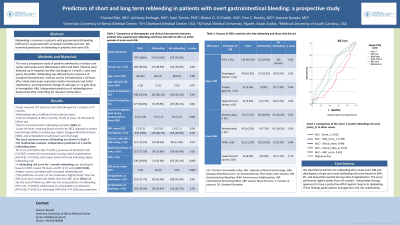
Results: 797 patients with GIB were followed-up for a median of 57 months. Rebleeding rates were 5.3% (in-hospital), 8.9% (1 month), 16.2% (1 year), and 21.8% (end of follow-up). On bivariate analysis, rebleeding was associated with lower Hb level, receiving blood transfusion (BT), stigmata of recent hemorrhage (SRH) on endoscopy, higher Glasgow-Blatchford Score (GBS), and antithrombotics on admission and discharge (Table 1). Independent predictors of 1-month rebleeding were BT of ≥3 units (HR=1.86; P=0.041), the presence of SRH (HR=1.99; P=0.007) and lowest Hb concentration reached during index hospitalization (HR=0.82; P=0.018), with a lower lowest Hb being predictive of higher rebleeding risk. We developed a rebleeding risk score based on SRH, lowest Hb level, and BT of ≥3 units, which had a satisfactory performance (AUC=0.68), and higher scores correlated with increased rebleeding risk. The model had a slightly better predictive accuracy [AUC=0.63, 95%CI 0.54-0.73), p=0.008] than the GBS (AUC=0.58, p=0.087), and the ABC score (AUC=0.62, p=0.012). By the end of follow-up, SRH was the only predictor of rebleeding (HR=1.61; P=0.003), while being on antiplatelet on admission (HR=0.66; P=0.021) or discharge (HR = 0.63; P=0.026) was protective against rebleeding.
Discussion: We identified risk factors for rebleeding after acute overt GIB and developed a simple and novel rebleeding risk score based on SRH, BT, and lowest Hb reached during index hospitalization. The score performed slightly better than risk models. Antiplatelet therapy appeared to have a protective effect against long-term rebleeding. These findings guide patient management and risk stratification.
Disclosures:
Chantal Rizk, MD1, Anthony Kerbage, MD2, Hani Tamim, PhD1, Walaa G. El Sheikh, BA1, Don C. Rockey, MD3, Kassem Barada, MD1. P3449 - Predictors of Short and Long Term Rebleeding in Patients with Overt Gastrointestinal Bleeding: A Prospective Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1American University of Beirut, Beirut, Beyrouth, Lebanon; 2Cleveland Clinic, Cleveland, OH; 3Medical University of South Carolina, Charleston, SC
Introduction: Rebleeding is common in patients with gastrointestinal bleeding (GIB) and is associated with increased morbidity and cost. We examined predictors of rebleeding in patients with overt GIB.
Methods: This was a prospective study of patients admitted to a tertiary care center with acute overt GIB between 2013 and 2023. Patients were followed-up in-hospital and after discharge at 1 month, 1 year and yearly thereafter. Rebleeding was defined by the presence of visualized hematemesis, melena, and/or hematochezia ≥ 24 hours after initial endoscopic evaluation and/or hemostasis and initial stabilization, accompanied by change of vital signs or ≥2 g/dL drop in hemoglobin (Hb). Independent predictors of rebleeding were determined after controlling for relevant confounders.
Results: 797 patients with GIB were followed-up for a median of 57 months. Rebleeding rates were 5.3% (in-hospital), 8.9% (1 month), 16.2% (1 year), and 21.8% (end of follow-up). On bivariate analysis, rebleeding was associated with lower Hb level, receiving blood transfusion (BT), stigmata of recent hemorrhage (SRH) on endoscopy, higher Glasgow-Blatchford Score (GBS), and antithrombotics on admission and discharge (Table 1). Independent predictors of 1-month rebleeding were BT of ≥3 units (HR=1.86; P=0.041), the presence of SRH (HR=1.99; P=0.007) and lowest Hb concentration reached during index hospitalization (HR=0.82; P=0.018), with a lower lowest Hb being predictive of higher rebleeding risk. We developed a rebleeding risk score based on SRH, lowest Hb level, and BT of ≥3 units, which had a satisfactory performance (AUC=0.68), and higher scores correlated with increased rebleeding risk. The model had a slightly better predictive accuracy [AUC=0.63, 95%CI 0.54-0.73), p=0.008] than the GBS (AUC=0.58, p=0.087), and the ABC score (AUC=0.62, p=0.012). By the end of follow-up, SRH was the only predictor of rebleeding (HR=1.61; P=0.003), while being on antiplatelet on admission (HR=0.66; P=0.021) or discharge (HR = 0.63; P=0.026) was protective against rebleeding.
Discussion: We identified risk factors for rebleeding after acute overt GIB and developed a simple and novel rebleeding risk score based on SRH, BT, and lowest Hb reached during index hospitalization. The score performed slightly better than risk models. Antiplatelet therapy appeared to have a protective effect against long-term rebleeding. These findings guide patient management and risk stratification.
Disclosures:
Chantal Rizk indicated no relevant financial relationships.
Anthony Kerbage indicated no relevant financial relationships.
Hani Tamim indicated no relevant financial relationships.
Walaa G. El Sheikh indicated no relevant financial relationships.
Don C. Rockey indicated no relevant financial relationships.
Kassem Barada indicated no relevant financial relationships.
Chantal Rizk, MD1, Anthony Kerbage, MD2, Hani Tamim, PhD1, Walaa G. El Sheikh, BA1, Don C. Rockey, MD3, Kassem Barada, MD1. P3449 - Predictors of Short and Long Term Rebleeding in Patients with Overt Gastrointestinal Bleeding: A Prospective Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
