Tuesday Poster Session
Category: GI Bleeding
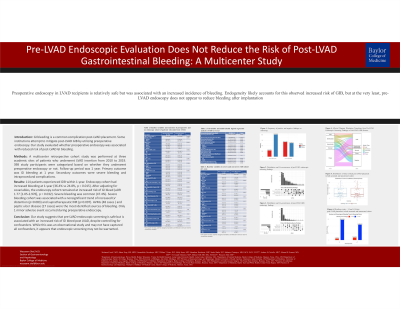
P3452 - Endoscopic Screening and the Risk of Post Left Ventricular Assist Device Gastrointestinal Bleeding: A Multicenter Retrospective Cohort Study
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
Wasseem Skef, MD
Baylor College of Medicine
Houston, TX
Presenting Author(s)
Award: Presidential Poster Award
Mohamed Azab, MD1, Jiahao Peng, MD, MPH2, Samanthika S. Devalaraju, MD3, William T. Cates, DO3, Molly Stone, MD4, Jonathan Reichstein, MD5, Sneha Shaha, DO6, Subhasis Chatterjee, MD3, Andrew B. Civitello, MD7, Mourad H. Senussi, MD, MS3, B. Joseph Elmunzer, MD, MSc8, Michael Volk, MD9, Wasseem Skef, MD3
1Prevea Health, Hobart, WI; 2Loma Linda University Health, Loma Linda, CA; 3Baylor College of Medicine, Houston, TX; 4University of Michigan, Ann Arbor, MI; 5Medical University of South Carolina, Charleston, SC; 6Loma Linda University Medical Center, Loma Linda, CA; 7Baylor College of Medicine/Texas Heart Institute, Houston, TN; 8Medical University of South Carolina, Mount Pleasant, SC; 9Loma Linda University, San Bernardino, CA
Introduction: LVADs are increasingly used as life prolonging therapy in advanced heart failure. Unfortunately, post LVAD GI hemorrhage is a common complication, contributing to morbidity and increased healthcare costs. Some centers attempt to mitigate bleeding by utilizing preoperative endoscopic screening; however, the evidence to support this practice is scant. Our study aimed to evaluate whether preoperative screening endoscopy was associated with reduced risk of post-LVAD GI bleeding.
Methods: A multicenter retrospective cohort study was performed at three academic sites of patients who underwent LVAD insertion from 2010 to 2019. Study participants were categorized based on whether they underwent preoperative screening endoscopy or not. Patients were followed for a year after insertion and various outcomes were collected. Primary outcome was bleeding at 1 year. Secondary outcomes were severe bleeding and intraprocedural complications. 398 patients met inclusion criteria. Baseline patient characteristics were compared by using the chi-square test for categorical variables and Wilcoxon rank sum test for continuous variables. Univariable and multivariable logistic regression analyses were performed for primary and secondary endpoints. All P values were two-tailed, with statistical significance thresholds set at p < 0.05. All statistical analyses were performed using SAS Software (version 9.4; SAS Institute Inc. Cary, NC, USA).
Results: Screening cohort had increased bleeding at 1-year (36.2% v 25%, p = 0.019). After adjusting for covariables (age, race, history of GI bleed, CAD, CKD, RV dysfunction, center, PPI use & anticoagulant use) screening cohort remained at increased risk of GI bleed (aOR 1.719 [1.018-2.901], p = 0.0425). Severe bleeding was common (47.4%). Severe bleeding cohort was associated with a borderline-significant trend towards increased LV distention (p=0.083) and supratherapeutic INR (p=0.097). AVMs (55.5%) and peptic ulcer disease (37.5%) were the most common identified source of bleeding. Only 1 complication was reported with screening endoscopy.
Discussion: Our study suggests that pre-LVAD endoscopic screening is safe, but increases rather than decreases risk of GI bleed post LVAD, despite controlling for known confounders. While this was an observational study and thus may not have captured all confounders, it appears that endoscopic screening may not be warranted.

Disclosures:
Mohamed Azab, MD1, Jiahao Peng, MD, MPH2, Samanthika S. Devalaraju, MD3, William T. Cates, DO3, Molly Stone, MD4, Jonathan Reichstein, MD5, Sneha Shaha, DO6, Subhasis Chatterjee, MD3, Andrew B. Civitello, MD7, Mourad H. Senussi, MD, MS3, B. Joseph Elmunzer, MD, MSc8, Michael Volk, MD9, Wasseem Skef, MD3. P3452 - Endoscopic Screening and the Risk of Post Left Ventricular Assist Device Gastrointestinal Bleeding: A Multicenter Retrospective Cohort Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Mohamed Azab, MD1, Jiahao Peng, MD, MPH2, Samanthika S. Devalaraju, MD3, William T. Cates, DO3, Molly Stone, MD4, Jonathan Reichstein, MD5, Sneha Shaha, DO6, Subhasis Chatterjee, MD3, Andrew B. Civitello, MD7, Mourad H. Senussi, MD, MS3, B. Joseph Elmunzer, MD, MSc8, Michael Volk, MD9, Wasseem Skef, MD3
1Prevea Health, Hobart, WI; 2Loma Linda University Health, Loma Linda, CA; 3Baylor College of Medicine, Houston, TX; 4University of Michigan, Ann Arbor, MI; 5Medical University of South Carolina, Charleston, SC; 6Loma Linda University Medical Center, Loma Linda, CA; 7Baylor College of Medicine/Texas Heart Institute, Houston, TN; 8Medical University of South Carolina, Mount Pleasant, SC; 9Loma Linda University, San Bernardino, CA
Introduction: LVADs are increasingly used as life prolonging therapy in advanced heart failure. Unfortunately, post LVAD GI hemorrhage is a common complication, contributing to morbidity and increased healthcare costs. Some centers attempt to mitigate bleeding by utilizing preoperative endoscopic screening; however, the evidence to support this practice is scant. Our study aimed to evaluate whether preoperative screening endoscopy was associated with reduced risk of post-LVAD GI bleeding.
Methods: A multicenter retrospective cohort study was performed at three academic sites of patients who underwent LVAD insertion from 2010 to 2019. Study participants were categorized based on whether they underwent preoperative screening endoscopy or not. Patients were followed for a year after insertion and various outcomes were collected. Primary outcome was bleeding at 1 year. Secondary outcomes were severe bleeding and intraprocedural complications. 398 patients met inclusion criteria. Baseline patient characteristics were compared by using the chi-square test for categorical variables and Wilcoxon rank sum test for continuous variables. Univariable and multivariable logistic regression analyses were performed for primary and secondary endpoints. All P values were two-tailed, with statistical significance thresholds set at p < 0.05. All statistical analyses were performed using SAS Software (version 9.4; SAS Institute Inc. Cary, NC, USA).
Results: Screening cohort had increased bleeding at 1-year (36.2% v 25%, p = 0.019). After adjusting for covariables (age, race, history of GI bleed, CAD, CKD, RV dysfunction, center, PPI use & anticoagulant use) screening cohort remained at increased risk of GI bleed (aOR 1.719 [1.018-2.901], p = 0.0425). Severe bleeding was common (47.4%). Severe bleeding cohort was associated with a borderline-significant trend towards increased LV distention (p=0.083) and supratherapeutic INR (p=0.097). AVMs (55.5%) and peptic ulcer disease (37.5%) were the most common identified source of bleeding. Only 1 complication was reported with screening endoscopy.
Discussion: Our study suggests that pre-LVAD endoscopic screening is safe, but increases rather than decreases risk of GI bleed post LVAD, despite controlling for known confounders. While this was an observational study and thus may not have captured all confounders, it appears that endoscopic screening may not be warranted.

Figure: Alluvial Diagram of Screening Endoscopic Findings and Post Endoscopic Findings in LVAD Patients Presenting with GI Bleed
Disclosures:
Mohamed Azab indicated no relevant financial relationships.
Jiahao Peng indicated no relevant financial relationships.
Samanthika Devalaraju indicated no relevant financial relationships.
William Cates indicated no relevant financial relationships.
Molly Stone indicated no relevant financial relationships.
Jonathan Reichstein indicated no relevant financial relationships.
Sneha Shaha indicated no relevant financial relationships.
Subhasis Chatterjee: Eagle Pharmaceutcials – Advisor or Review Panel Member.
Andrew Civitello indicated no relevant financial relationships.
Mourad Senussi indicated no relevant financial relationships.
B. Joseph Elmunzer indicated no relevant financial relationships.
Michael Volk: Bausch Health – Consultant, Speakers Bureau. Biovie – Consultant. Boston Scientific – Consultant.
Wasseem Skef: GE Healthcare – Stock-publicly held company(excluding mutual/index funds).
Mohamed Azab, MD1, Jiahao Peng, MD, MPH2, Samanthika S. Devalaraju, MD3, William T. Cates, DO3, Molly Stone, MD4, Jonathan Reichstein, MD5, Sneha Shaha, DO6, Subhasis Chatterjee, MD3, Andrew B. Civitello, MD7, Mourad H. Senussi, MD, MS3, B. Joseph Elmunzer, MD, MSc8, Michael Volk, MD9, Wasseem Skef, MD3. P3452 - Endoscopic Screening and the Risk of Post Left Ventricular Assist Device Gastrointestinal Bleeding: A Multicenter Retrospective Cohort Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

