Tuesday Poster Session
Category: GI Bleeding
P3462 - Clinical Efficacy of Video Capsule Endoscopy and Balloon-Assisted in Suspected Small Bowel Bleeding: A Single Center Cohort Study
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- SE
Sandra Elmasry, MD
Mayo Clinic College of Medicine
Scottsdale, Arizona
Presenting Author(s)
Sandra Elmasry, MD1, Kevin Song, MD2, Jacyln Tuck, MB, BCh, MA3, Blanca Lizaola-Mayo, MD4, Kevin Ruff, MD5, Shabana Pasha, MD1, Jonathan Leighton, MD1
1Mayo Clinic College of Medicine, Scottsdale, AZ; 2Mayo Clinic College of Medicine, Bellevue, WA; 3Mayo Clinic Arizona, Scottsdale, AZ; 4Mayo Clinic, Phoenix, AZ; 5Mayo Clinic, Scottsdale, AZ
Introduction: While video endoscopy capsule (VCE) and balloon assisted enteroscopy (BAE) have emerged as the gold standard for the evaluation and treatment of suspected small bowel bleeds (SSBB), little is known regarding the clinical efficacy when used in combination. We aim to assess diagnostic yields [DY] and inter-modality agreement between VCE and BAE in SSBB.
Methods: Patients who underwent VCE followed by BAE from 2012 to 2022 for SSBB were prospectivelt identified. Patients with incomplete study or waiting interval between VCE and BAE > 12 months were excluded. Clinical characteristics were collected via chart review. Diagnostic yield (DY) was defined as the proportion of positive test per the Saurin classification. Waiting interval between VCE and BAE was considered short if within 30 days and long if after 30 days. Inter-modality agreement was obtained by calculating Cohen’s kappa (k) co-efficient. The agreement obtained was considered slight (k = 0.00–0.20), fair (k = 0.21–0.40), moderate (k = 0.41–0.60), substantial (k = 0.61–0.80), or almost perfect (k = 0.81–1.00). Continuous and categorical values were assessed with Fisher’s or T-test when appropriate
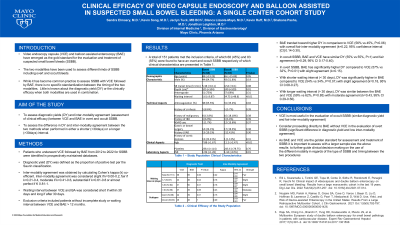
Results: 151 patients met the inclusion criteria, of which 68 (45%) and 83 (55%) were found to have an overt and occult SSBB respectively. Patient outcomes are described in Table 1. Overall, BAE trended toward higher DY in comparison to VCE (56% vs 45%, P=0.06) with overall fair inter-modality agreement (k=0.22) In patients with shorter waiting interval (< 30 days), DY was significantly higher in BAE compared to VCE (54% vs 34%, P=0.01) with slight agreement (k=0.18). In patients with longer waiting interval ( > 30 days), DY was similar between the BAE and VCE (59% vs 62%, P=0.85) with moderate agreement (k=0.43) In patients with occult SSBB, BAE and VCE have similar DY (55% vs 55%, P=1) and fair agreement (k=0.29). In overt SSBB group, BAE has significantly higher DY compared to VCE (57% vs 32%, P=0.01) with slight agreement (k=0.15).
Discussion: Compared to VCE, DY of BAE is significantly higher in overt SSBB and shorter waiting interval. Inter-modality agreement is better in occult SSBB and longer waiting intervals. DY of BAE and inter-modality agreement appear to be inversely related with respect to time and subtypes of SSBB. A larger sample size and additional studies are needed to confirm the results and provide guidance for clinical practice.
Disclosures:
Sandra Elmasry, MD1, Kevin Song, MD2, Jacyln Tuck, MB, BCh, MA3, Blanca Lizaola-Mayo, MD4, Kevin Ruff, MD5, Shabana Pasha, MD1, Jonathan Leighton, MD1. P3462 - Clinical Efficacy of Video Capsule Endoscopy and Balloon-Assisted in Suspected Small Bowel Bleeding: A Single Center Cohort Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Mayo Clinic College of Medicine, Scottsdale, AZ; 2Mayo Clinic College of Medicine, Bellevue, WA; 3Mayo Clinic Arizona, Scottsdale, AZ; 4Mayo Clinic, Phoenix, AZ; 5Mayo Clinic, Scottsdale, AZ
Introduction: While video endoscopy capsule (VCE) and balloon assisted enteroscopy (BAE) have emerged as the gold standard for the evaluation and treatment of suspected small bowel bleeds (SSBB), little is known regarding the clinical efficacy when used in combination. We aim to assess diagnostic yields [DY] and inter-modality agreement between VCE and BAE in SSBB.
Methods: Patients who underwent VCE followed by BAE from 2012 to 2022 for SSBB were prospectivelt identified. Patients with incomplete study or waiting interval between VCE and BAE > 12 months were excluded. Clinical characteristics were collected via chart review. Diagnostic yield (DY) was defined as the proportion of positive test per the Saurin classification. Waiting interval between VCE and BAE was considered short if within 30 days and long if after 30 days. Inter-modality agreement was obtained by calculating Cohen’s kappa (k) co-efficient. The agreement obtained was considered slight (k = 0.00–0.20), fair (k = 0.21–0.40), moderate (k = 0.41–0.60), substantial (k = 0.61–0.80), or almost perfect (k = 0.81–1.00). Continuous and categorical values were assessed with Fisher’s or T-test when appropriate
Results: 151 patients met the inclusion criteria, of which 68 (45%) and 83 (55%) were found to have an overt and occult SSBB respectively. Patient outcomes are described in Table 1. Overall, BAE trended toward higher DY in comparison to VCE (56% vs 45%, P=0.06) with overall fair inter-modality agreement (k=0.22) In patients with shorter waiting interval (< 30 days), DY was significantly higher in BAE compared to VCE (54% vs 34%, P=0.01) with slight agreement (k=0.18). In patients with longer waiting interval ( > 30 days), DY was similar between the BAE and VCE (59% vs 62%, P=0.85) with moderate agreement (k=0.43) In patients with occult SSBB, BAE and VCE have similar DY (55% vs 55%, P=1) and fair agreement (k=0.29). In overt SSBB group, BAE has significantly higher DY compared to VCE (57% vs 32%, P=0.01) with slight agreement (k=0.15).
Discussion: Compared to VCE, DY of BAE is significantly higher in overt SSBB and shorter waiting interval. Inter-modality agreement is better in occult SSBB and longer waiting intervals. DY of BAE and inter-modality agreement appear to be inversely related with respect to time and subtypes of SSBB. A larger sample size and additional studies are needed to confirm the results and provide guidance for clinical practice.
Disclosures:
Sandra Elmasry indicated no relevant financial relationships.
Kevin Song indicated no relevant financial relationships.
Jacyln Tuck indicated no relevant financial relationships.
Blanca Lizaola-Mayo indicated no relevant financial relationships.
Kevin Ruff indicated no relevant financial relationships.
Shabana Pasha: abbvie – Grant/Research Support. medtronic – Grant/Research Support.
Jonathan Leighton: ANX – Advisor or Review Panel Member. Braintree – Advisor or Review Panel Member. Fresenius Kabi – Advisor or Review Panel Member. SEI Healthcare – Advisor or Review Panel Member.
Sandra Elmasry, MD1, Kevin Song, MD2, Jacyln Tuck, MB, BCh, MA3, Blanca Lizaola-Mayo, MD4, Kevin Ruff, MD5, Shabana Pasha, MD1, Jonathan Leighton, MD1. P3462 - Clinical Efficacy of Video Capsule Endoscopy and Balloon-Assisted in Suspected Small Bowel Bleeding: A Single Center Cohort Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
