Tuesday Poster Session
Category: GI Bleeding
P3468 - Mysterious Lower GI Bleed Due to Splenic Artery-Colonic Fistula; Rare Case Report and Review of Literature
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Robert J. Pattison, MD
Sunrise Health Gastroenterology Fellowship
Las Vegas, NV
Presenting Author(s)
Robert Pattison, MD1, George Trad, MD2, Victoria Diaz, MD2, Tomoki Sempokuya, MD3, Syed Abdul Basit, MD4, John Ryan, MD4
1Sunrise Health Gastroenterology Fellowship, Las Vegas, NV; 2Sunrise Health GME Consortium, Las Vegas, NV; 3University of Nebraska Medical Center, Honolulu, HI; 4Southern Hills Medical Center, Las Vegas, NV
Introduction: Splenic artery aneurysm can be a result of portal hypertension which can invade local
surrounding structure leading to complications such as splenic artery-colonic fistula. Splenic
artery-colonic fistulizations is an exceedingly rare phenomenon that can result in a massive GI
bleed that is extremely fatal if not diagnosed accurately and promptly. Our case report explains
the importance of broader differential diagnosis for patients presenting with hematochezia as
well the importance of detailed medical history. Only six cases were reported in the past with
similar presentations in English literature [table 1].
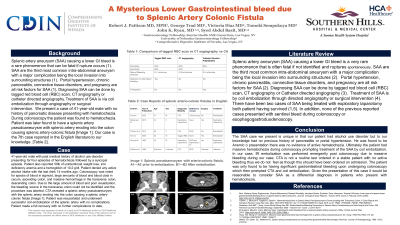
Case Description/Methods: 41-year-old male with past medical history of alcohol use disorder and esophageal varices
presenting for four episodes of hematochezia followed by a syncopal episode. Patient also
reported 50lb of unintentional weight loss. Patient denies any active alcohol intake with the last
drink 14 months ago. Colonoscopy was noted for specks of blood in sigmoid, large amounts of
blood and blood clots in cecum, ascending colon, transverse colon, descending colon. Due to the
large amount of blood and poor visualization, the bleeding source in the transverse colon could
not be identified. CTA revealed a splenic artery pseudoaneurysm with the splenic artery eroding
into the colon causing a splenic artery-colonic fistula [Figure 1]. Patient was resuscitated and
underwent successful coil embolization of the splenic artery with no complications. Patient made
a full recovery with no further complications to date.
Discussion: SAA are the third most common intra-abdominal aneurysm, a major complication of which
being the invasion of into local anatomy. Risk factors for the development of SAA include portal
hypertension, chronic pancreatitis, connective tissue disorders, and pregnancy. Diagnosing SAA
can be done by utilizing a tagged red blood cell (RBC) scan, computed tomography angiography
(CTA) or catheter directed angiography. Treatment of SAA is by coil embolization through
directed angiography or surgical intervention. SAA should be suspected in patients who present
with hematochezia who continue to have overt GI bleeding after a negative EGD and
colonoscopy evaluation.
Disclosures:
Robert Pattison, MD1, George Trad, MD2, Victoria Diaz, MD2, Tomoki Sempokuya, MD3, Syed Abdul Basit, MD4, John Ryan, MD4. P3468 - Mysterious Lower GI Bleed Due to Splenic Artery-Colonic Fistula; Rare Case Report and Review of Literature, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Sunrise Health Gastroenterology Fellowship, Las Vegas, NV; 2Sunrise Health GME Consortium, Las Vegas, NV; 3University of Nebraska Medical Center, Honolulu, HI; 4Southern Hills Medical Center, Las Vegas, NV
Introduction: Splenic artery aneurysm can be a result of portal hypertension which can invade local
surrounding structure leading to complications such as splenic artery-colonic fistula. Splenic
artery-colonic fistulizations is an exceedingly rare phenomenon that can result in a massive GI
bleed that is extremely fatal if not diagnosed accurately and promptly. Our case report explains
the importance of broader differential diagnosis for patients presenting with hematochezia as
well the importance of detailed medical history. Only six cases were reported in the past with
similar presentations in English literature [table 1].
Case Description/Methods: 41-year-old male with past medical history of alcohol use disorder and esophageal varices
presenting for four episodes of hematochezia followed by a syncopal episode. Patient also
reported 50lb of unintentional weight loss. Patient denies any active alcohol intake with the last
drink 14 months ago. Colonoscopy was noted for specks of blood in sigmoid, large amounts of
blood and blood clots in cecum, ascending colon, transverse colon, descending colon. Due to the
large amount of blood and poor visualization, the bleeding source in the transverse colon could
not be identified. CTA revealed a splenic artery pseudoaneurysm with the splenic artery eroding
into the colon causing a splenic artery-colonic fistula [Figure 1]. Patient was resuscitated and
underwent successful coil embolization of the splenic artery with no complications. Patient made
a full recovery with no further complications to date.
Discussion: SAA are the third most common intra-abdominal aneurysm, a major complication of which
being the invasion of into local anatomy. Risk factors for the development of SAA include portal
hypertension, chronic pancreatitis, connective tissue disorders, and pregnancy. Diagnosing SAA
can be done by utilizing a tagged red blood cell (RBC) scan, computed tomography angiography
(CTA) or catheter directed angiography. Treatment of SAA is by coil embolization through
directed angiography or surgical intervention. SAA should be suspected in patients who present
with hematochezia who continue to have overt GI bleeding after a negative EGD and
colonoscopy evaluation.
Disclosures:
Robert Pattison indicated no relevant financial relationships.
George Trad indicated no relevant financial relationships.
Victoria Diaz indicated no relevant financial relationships.
Tomoki Sempokuya indicated no relevant financial relationships.
Syed Abdul Basit indicated no relevant financial relationships.
John Ryan indicated no relevant financial relationships.
Robert Pattison, MD1, George Trad, MD2, Victoria Diaz, MD2, Tomoki Sempokuya, MD3, Syed Abdul Basit, MD4, John Ryan, MD4. P3468 - Mysterious Lower GI Bleed Due to Splenic Artery-Colonic Fistula; Rare Case Report and Review of Literature, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
