Tuesday Poster Session
Category: GI Bleeding
P3473 - Disseminated Histoplasmosis: A Gastrointestinal Manifestation
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Oluwaposi Omiwade, MD
Scripps Mercy Hospital
San Diego, CA
Presenting Author(s)
Oluwaposi Omiwade, MD
Scripps Mercy Hospital, San Diego, CA
Introduction: This is a rare case of GI bleeding and management of a clinically unstable patient with HIV/AIDS who was diagnosed with disseminated histoplasmosis (DH).
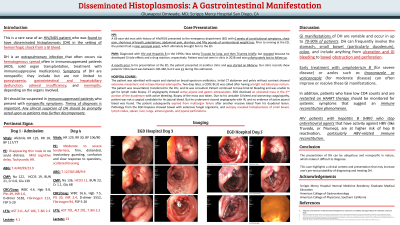
Case Description/Methods: A 63-year-old man with history of HIV presented with 6 weeks of constitutional symptoms, chest pain, shortness of breath, palpitations, abdominal pain, diarrhea, and fifty pounds of weight loss. The patient was diagnosed with HIV and Hepatitis B (HBV) in the 1990s; he had taken Truvada and Triumeq but stopped because he developed GI side effects and a drug reaction, respectively. One month before his presentation, the patient was started on Biktarvy. CD4 count was 21. The patient was admitted with sepsis and started on broad-spectrum antibiotics. Initial CT abdomen and pelvis without contrast showed extensive mesenteric and retroperitoneal adenopathy. Two days later, a code blue was called after the patient had bloody bowel movement. The patient was resuscitated, transferred to the ICU, and intubated. The patient continued to have brisk GI bleeding despite transfusion. CT angiography showed active jejunal and gastric extravasation. EGD disclosed an ulcerated mass in the 2nd portion of the duodenum with active bleeding. Biopsy of the mass was taken. Due to his unstable GI bleed and worsening coagulopathy, patient was not a surgical candidate for his jejunal bleed. The patient subsequently expired from multiorgan failure after another massive bleed from his duodenal lesion. Pathology from the EGD biopsies showed bowel with extensive fungal organisms, and autopsy revealed histoplasmosis of small bowel, lymph nodes, spleen, liver, lungs, and adrenal glands.
Discussion: Symptoms of DH are broad and variable; they include but are not limited to GI and hepatobiliary dysfunction, pancytopenia, adrenal insufficiency, and CNS disease. DH should be suspected in severely immunosuppressed patients (such as patients with low CD4 count) with nonspecific, multisystemic symptoms. GI bleed and clinical instability may preclude tissue diagnosis, but Histoplasma urine antigen and fungal serologies may be a reasonable option. In addition, patients who have low CD4 counts and are restarted on HAART therapy (such as Biktarvy) should be monitored for symptoms that suggest an immune reconstitution phenomenon. It is important to note that HIV patients with HBV who stop antiretroviral agents that have activity against HBV (like Truvada, or Triumeq), are at higher risk of hep B reactivation, particularly HBV-related immune reconstitution.

Disclosures:
Oluwaposi Omiwade, MD. P3473 - Disseminated Histoplasmosis: A Gastrointestinal Manifestation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Scripps Mercy Hospital, San Diego, CA
Introduction: This is a rare case of GI bleeding and management of a clinically unstable patient with HIV/AIDS who was diagnosed with disseminated histoplasmosis (DH).
Case Description/Methods: A 63-year-old man with history of HIV presented with 6 weeks of constitutional symptoms, chest pain, shortness of breath, palpitations, abdominal pain, diarrhea, and fifty pounds of weight loss. The patient was diagnosed with HIV and Hepatitis B (HBV) in the 1990s; he had taken Truvada and Triumeq but stopped because he developed GI side effects and a drug reaction, respectively. One month before his presentation, the patient was started on Biktarvy. CD4 count was 21. The patient was admitted with sepsis and started on broad-spectrum antibiotics. Initial CT abdomen and pelvis without contrast showed extensive mesenteric and retroperitoneal adenopathy. Two days later, a code blue was called after the patient had bloody bowel movement. The patient was resuscitated, transferred to the ICU, and intubated. The patient continued to have brisk GI bleeding despite transfusion. CT angiography showed active jejunal and gastric extravasation. EGD disclosed an ulcerated mass in the 2nd portion of the duodenum with active bleeding. Biopsy of the mass was taken. Due to his unstable GI bleed and worsening coagulopathy, patient was not a surgical candidate for his jejunal bleed. The patient subsequently expired from multiorgan failure after another massive bleed from his duodenal lesion. Pathology from the EGD biopsies showed bowel with extensive fungal organisms, and autopsy revealed histoplasmosis of small bowel, lymph nodes, spleen, liver, lungs, and adrenal glands.
Discussion: Symptoms of DH are broad and variable; they include but are not limited to GI and hepatobiliary dysfunction, pancytopenia, adrenal insufficiency, and CNS disease. DH should be suspected in severely immunosuppressed patients (such as patients with low CD4 count) with nonspecific, multisystemic symptoms. GI bleed and clinical instability may preclude tissue diagnosis, but Histoplasma urine antigen and fungal serologies may be a reasonable option. In addition, patients who have low CD4 counts and are restarted on HAART therapy (such as Biktarvy) should be monitored for symptoms that suggest an immune reconstitution phenomenon. It is important to note that HIV patients with HBV who stop antiretroviral agents that have activity against HBV (like Truvada, or Triumeq), are at higher risk of hep B reactivation, particularly HBV-related immune reconstitution.

Figure: Patient's EGD which showed ulcerated mass with active bleeding in the 2nd portion of duodenum.
Disclosures:
Oluwaposi Omiwade indicated no relevant financial relationships.
Oluwaposi Omiwade, MD. P3473 - Disseminated Histoplasmosis: A Gastrointestinal Manifestation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

