Tuesday Poster Session
Category: GI Bleeding
P3475 - When the Order of Events Is Not the Usual One: A Curious Case of Ulcerative Colitis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Jose F. Nunez-Morales, MD
VA Caribbean Healthcare System
San Juan, PR
Presenting Author(s)
Jose F.. Nunez-Morales, MD, Diego Roman-Colon, MD, Pedro Rosa-Cortes, MD, Loscar Santiago-Rivera, MD, Jose Martin-Ortiz, MD, FACG
VA Caribbean Healthcare System, San Juan, Puerto Rico
Introduction: The incidence and prevalence of inflammatory bowel disease (IBD) is increasing globally and coupled with an ageing population, the number of elderly patients with IBD should continue this trend. The diagnosis of IBD in the elderly is often difficult and can easily be confused. It is also known that patients with IBD are at significantly increased risk of colorectal cancer; however, scarce literature is available describing IBD in patients with history of colorectal cancer. We present a curious case of a nonagenarian with previous history of colon adenocarcinoma that was diagnosed with Ulcerative Colitis.
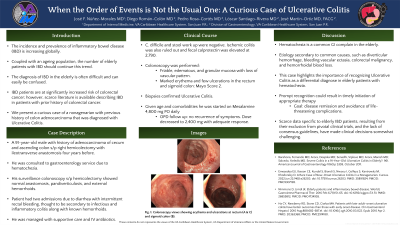
Case Description/Methods: A 91-year-old male with history of colorectal adenocarcinoma s/p right hemicolectomy with ileotransverse anastomosis four years before that was consulted to gastroenterology service due to hematochezia. His surveillance colonoscopy s/p hemicolectomy had shown normal anastomosis, pandiverticulosis, and external hemorrhoids. Patient had two admissions due to diarrhea with intermittent rectal bleeding, thought to be secondary to infectious and inflammatory colitis along with known hemorrhoids. He was managed with supportive care and IV antibiotics. C. difficile and stool work up were negative. Ischemic colitis was also ruled out. Fecal calprotectin was elevated at 2,790. A colonoscopy was recommended, which revealed a friable, edematous, and granular mucosa with loss of vascular pattern along with marked erythema and few ulcerations in the rectum and sigmoid colon (Mayo Score 2). Biopsies confirmed Ulcerative Colitis. Treatment options were discussed and given comorbidities and age, he was started on Mesalamine 4,800 mg PO daily with adequate response.
Discussion: Although hematochezia remains the most frequently described clinical finding in the elderly, it is commonly presumed to be secondary to more common causes, such as diverticular hemorrhage, bleeding vascular ectasia, colorectal malignancy, and hemorrhoidal blood loss. This case highlights the importance of recognizing Ulcerative Colitis as one of the differential diagnoses in elderly patients presenting with hematochezia. Prompt recognition could result in timely initiation of appropriate therapy, leading to disease remission and avoidance of life-threatening complications. In addition, the scarce data specific to elderly IBD patients often resulting from their exclusion from pivotal clinical trials and the lack of consensus guidelines, have made clinical decisions somewhat challenging.
Disclosures:
Jose F.. Nunez-Morales, MD, Diego Roman-Colon, MD, Pedro Rosa-Cortes, MD, Loscar Santiago-Rivera, MD, Jose Martin-Ortiz, MD, FACG. P3475 - When the Order of Events Is Not the Usual One: A Curious Case of Ulcerative Colitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
VA Caribbean Healthcare System, San Juan, Puerto Rico
Introduction: The incidence and prevalence of inflammatory bowel disease (IBD) is increasing globally and coupled with an ageing population, the number of elderly patients with IBD should continue this trend. The diagnosis of IBD in the elderly is often difficult and can easily be confused. It is also known that patients with IBD are at significantly increased risk of colorectal cancer; however, scarce literature is available describing IBD in patients with history of colorectal cancer. We present a curious case of a nonagenarian with previous history of colon adenocarcinoma that was diagnosed with Ulcerative Colitis.
Case Description/Methods: A 91-year-old male with history of colorectal adenocarcinoma s/p right hemicolectomy with ileotransverse anastomosis four years before that was consulted to gastroenterology service due to hematochezia. His surveillance colonoscopy s/p hemicolectomy had shown normal anastomosis, pandiverticulosis, and external hemorrhoids. Patient had two admissions due to diarrhea with intermittent rectal bleeding, thought to be secondary to infectious and inflammatory colitis along with known hemorrhoids. He was managed with supportive care and IV antibiotics. C. difficile and stool work up were negative. Ischemic colitis was also ruled out. Fecal calprotectin was elevated at 2,790. A colonoscopy was recommended, which revealed a friable, edematous, and granular mucosa with loss of vascular pattern along with marked erythema and few ulcerations in the rectum and sigmoid colon (Mayo Score 2). Biopsies confirmed Ulcerative Colitis. Treatment options were discussed and given comorbidities and age, he was started on Mesalamine 4,800 mg PO daily with adequate response.
Discussion: Although hematochezia remains the most frequently described clinical finding in the elderly, it is commonly presumed to be secondary to more common causes, such as diverticular hemorrhage, bleeding vascular ectasia, colorectal malignancy, and hemorrhoidal blood loss. This case highlights the importance of recognizing Ulcerative Colitis as one of the differential diagnoses in elderly patients presenting with hematochezia. Prompt recognition could result in timely initiation of appropriate therapy, leading to disease remission and avoidance of life-threatening complications. In addition, the scarce data specific to elderly IBD patients often resulting from their exclusion from pivotal clinical trials and the lack of consensus guidelines, have made clinical decisions somewhat challenging.
Disclosures:
Jose Nunez-Morales indicated no relevant financial relationships.
Diego Roman-Colon indicated no relevant financial relationships.
Pedro Rosa-Cortes indicated no relevant financial relationships.
Loscar Santiago-Rivera indicated no relevant financial relationships.
Jose Martin-Ortiz indicated no relevant financial relationships.
Jose F.. Nunez-Morales, MD, Diego Roman-Colon, MD, Pedro Rosa-Cortes, MD, Loscar Santiago-Rivera, MD, Jose Martin-Ortiz, MD, FACG. P3475 - When the Order of Events Is Not the Usual One: A Curious Case of Ulcerative Colitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
