Tuesday Poster Session
Category: GI Bleeding
P3476 - Unraveling the Silent Strangler: Takayasu Arteritis Unleashing Hematochezia
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- MG
Mahathi Gangavarapu, BA
University of Missouri-Kansas City
Kansas City, MO
Presenting Author(s)
Award: Presidential Poster Award
Mahathi Gangavarapu, BA, Vinay Jahagirdar, MD, Prathishtha Pitchyaiah, BA, John P. Campbell, MD
University of Missouri-Kansas City, Kansas City, MO
Introduction: Takayasu arteritis (TA) is a large vessel vasculitis predominantly affecting young females. It is characterized by inflammation of the aorta and its branches, leading to manifestations such as limb claudication, vascular bruits, weight loss, fever, muscle/joint aches, and renovascular hypertension. Gradual vascular narrowing is common; rapid vascular occlusion leading to chronic or critical ischemia is less common. In this case report, we present a unique case of TA in a young male patient who developed chronic mesenteric ischemia and SMA/IMA thrombosis as a complication.
Case Description/Methods: A 38-year-old Burmese speaking man presented to the ED with large volume hematochezia, dizziness and dyspnea. Patient presented multiple times with similar episodes over 4 years. Despite recurrent transfusions and iron therapy, Hgb remained low. History was notable for TA complicated by SMA/IMA thrombosis, mesenteric ischemia, and stroke (treated with DAPT) and ischemic small bowel injury.
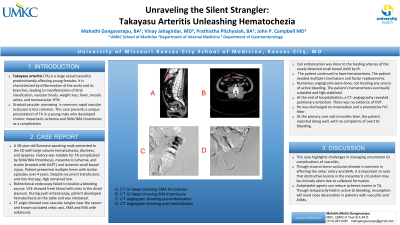
Bidirectional endoscopy failed to localize a bleeding source. VCE showed fresh blood with clots in the distal jejunum. During push enteroscopy, patient developed hematochezia on the table and was intubated. CT angio showed new vascular tangles near the cecum and known occluded celiac axis, SMA and IMA with collaterals. Coil embolization was done to the feeding arteries of the newly detected small bowel AVM by IR. However, the patient continued to have hematochezia. The patient needed multiple transfusions and factor replacements. Numerous angiograms were done, not locating any source of active bleeding. The patient’s hematochezia eventually subsided and Hgb stabilized. At the end of hospitalization, a CT-angio revealed pulmonary embolism. There was no evidence of DVT. He was discharged on rivaroxaban and a preemptive IVC filter. At the primary care visit 6 months later, the patient reported doing well, with no complaints of overt GI bleeding.
Discussion: The case highlights challenges in managing uncommon GI complications of vasculitis. The association between TA and IBD is well described; there are only sporadic cases documenting AV malformations in TA. Visceral steno-occlusive disease is common, with TA affecting the celiac artery and the SMA. Obstructive lesions in mesenteric circulation may be clinically silent due to collateral formation. Antiplatelet agents can reduce ischemic events in TA. Though temporarily held in active GI bleeding, resumption needs close observation in patients with vasculitis and AVMs.

Disclosures:
Mahathi Gangavarapu, BA, Vinay Jahagirdar, MD, Prathishtha Pitchyaiah, BA, John P. Campbell, MD. P3476 - Unraveling the Silent Strangler: Takayasu Arteritis Unleashing Hematochezia, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Mahathi Gangavarapu, BA, Vinay Jahagirdar, MD, Prathishtha Pitchyaiah, BA, John P. Campbell, MD
University of Missouri-Kansas City, Kansas City, MO
Introduction: Takayasu arteritis (TA) is a large vessel vasculitis predominantly affecting young females. It is characterized by inflammation of the aorta and its branches, leading to manifestations such as limb claudication, vascular bruits, weight loss, fever, muscle/joint aches, and renovascular hypertension. Gradual vascular narrowing is common; rapid vascular occlusion leading to chronic or critical ischemia is less common. In this case report, we present a unique case of TA in a young male patient who developed chronic mesenteric ischemia and SMA/IMA thrombosis as a complication.
Case Description/Methods: A 38-year-old Burmese speaking man presented to the ED with large volume hematochezia, dizziness and dyspnea. Patient presented multiple times with similar episodes over 4 years. Despite recurrent transfusions and iron therapy, Hgb remained low. History was notable for TA complicated by SMA/IMA thrombosis, mesenteric ischemia, and stroke (treated with DAPT) and ischemic small bowel injury.
Bidirectional endoscopy failed to localize a bleeding source. VCE showed fresh blood with clots in the distal jejunum. During push enteroscopy, patient developed hematochezia on the table and was intubated. CT angio showed new vascular tangles near the cecum and known occluded celiac axis, SMA and IMA with collaterals. Coil embolization was done to the feeding arteries of the newly detected small bowel AVM by IR. However, the patient continued to have hematochezia. The patient needed multiple transfusions and factor replacements. Numerous angiograms were done, not locating any source of active bleeding. The patient’s hematochezia eventually subsided and Hgb stabilized. At the end of hospitalization, a CT-angio revealed pulmonary embolism. There was no evidence of DVT. He was discharged on rivaroxaban and a preemptive IVC filter. At the primary care visit 6 months later, the patient reported doing well, with no complaints of overt GI bleeding.
Discussion: The case highlights challenges in managing uncommon GI complications of vasculitis. The association between TA and IBD is well described; there are only sporadic cases documenting AV malformations in TA. Visceral steno-occlusive disease is common, with TA affecting the celiac artery and the SMA. Obstructive lesions in mesenteric circulation may be clinically silent due to collateral formation. Antiplatelet agents can reduce ischemic events in TA. Though temporarily held in active GI bleeding, resumption needs close observation in patients with vasculitis and AVMs.

Figure: A: CT GI bleed showing SMA thrombosis; B: CT GI bleed showing IMA thrombosis; C: CT angiogram showing pre-embolization; D: CT angiogram showing post-embolization
Disclosures:
Mahathi Gangavarapu indicated no relevant financial relationships.
Vinay Jahagirdar indicated no relevant financial relationships.
Prathishtha Pitchyaiah indicated no relevant financial relationships.
John P. Campbell indicated no relevant financial relationships.
Mahathi Gangavarapu, BA, Vinay Jahagirdar, MD, Prathishtha Pitchyaiah, BA, John P. Campbell, MD. P3476 - Unraveling the Silent Strangler: Takayasu Arteritis Unleashing Hematochezia, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

