Tuesday Poster Session
Category: GI Bleeding
P3479 - Unique Case of Bleeding Barium Contrast Fecalith
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Shane Quo, DO
University of Miami at Holy Cross Hospital
Fort Lauderdale, FL
Presenting Author(s)
Shane Quo, DO1, Mary Parianos, MD2, Alyssa Benjamin, DO1, Charles Hotte, MD3
1University of Miami Holy Cross Hospital, Fort Lauderdale, FL; 2University of Miami Holy Cross, Fort Lauderdale, FL; 3Gastroenterology Institute of Fort Lauderdale and Holy Cross Hospital, Fort Lauderdale, FL
Introduction: Gastrointestinal bleeds are amongst the most common reasons for a patient to be hospitalized. The approach typically includes fluid resuscitation, proton pump inhibitor, and transfusion of packed red blood cells(pRBCs) as needed. However, it is essential for physicians to evaluate the cause and adapt their approach. We present a unique case of a gastrointestinal bleed as a result of a calcified barium fecalith.
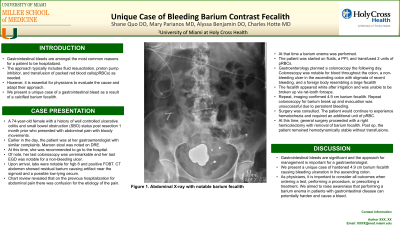
Case Description/Methods: A 74-year-old female with a history of well controlled ulcerative colitis and small bowel obstruction (SBO) status post resection 1 month prior who presented with abdominal pain with bloody movements. Earlier in the day, the patient was at her gastroenterologist with similar complaints. Maroon stool was noted on DRE. At this time, she was recommended to go to the hospital. Of note, her last colonoscopy was unremarkable and her last EGD was notable for a non-bleeding ulcer. Upon arrival, labs were notable for hgb 8 and positive FOBT. CT abdomen showed residual barium causing artifact near the sigmoid and a possible low-lying cecum. Chart review revealed that on the previous hospitalization for abdominal pain there was confusion for the etiology of the pain. At that time a barium enema was performed. The patient was started on fluids, a PPI, and transfused 2 units of pRBCs. Gastroenterology planned a colonoscopy the following day. Colonoscopy was notable for blood throughout the colon, a non-bleeding ulcer in the ascending colon with stigmata of recent bleeding, and a foreign body resembling a large fecalith (Figure 1/2). The fecalith appeared white after irrigation and was unable to be broken up via rat-tooth forceps. Repeat, imaging confirmed 4.9 cm barium fecalith. Repeat colonoscopy for barium break up and evacuation was unsuccessful due to persistent bleeding. Surgery was consulted. The patient would continue to experience hematochezia and required an additional unit of pRBC. At this time, surgery proceeded with a right hemicolectomy with removal of barium fecalith. Post op, the patient remained stable without transfusions.
Discussion: Gastrointestinal bleeds are significant and the approach for management is important. We present a unique case of hardened 4.9 cm barium fecalith causing bleeding ulceration in the ascending colon. As physicians, it is important to consider all outcomes when ordering a test, performing a procedure, or prescribing a treatment. We aimed to raise awareness that performing a simple test like a barium enema can even cause a bleed.

Disclosures:
Shane Quo, DO1, Mary Parianos, MD2, Alyssa Benjamin, DO1, Charles Hotte, MD3. P3479 - Unique Case of Bleeding Barium Contrast Fecalith, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Miami Holy Cross Hospital, Fort Lauderdale, FL; 2University of Miami Holy Cross, Fort Lauderdale, FL; 3Gastroenterology Institute of Fort Lauderdale and Holy Cross Hospital, Fort Lauderdale, FL
Introduction: Gastrointestinal bleeds are amongst the most common reasons for a patient to be hospitalized. The approach typically includes fluid resuscitation, proton pump inhibitor, and transfusion of packed red blood cells(pRBCs) as needed. However, it is essential for physicians to evaluate the cause and adapt their approach. We present a unique case of a gastrointestinal bleed as a result of a calcified barium fecalith.
Case Description/Methods: A 74-year-old female with a history of well controlled ulcerative colitis and small bowel obstruction (SBO) status post resection 1 month prior who presented with abdominal pain with bloody movements. Earlier in the day, the patient was at her gastroenterologist with similar complaints. Maroon stool was noted on DRE. At this time, she was recommended to go to the hospital. Of note, her last colonoscopy was unremarkable and her last EGD was notable for a non-bleeding ulcer. Upon arrival, labs were notable for hgb 8 and positive FOBT. CT abdomen showed residual barium causing artifact near the sigmoid and a possible low-lying cecum. Chart review revealed that on the previous hospitalization for abdominal pain there was confusion for the etiology of the pain. At that time a barium enema was performed. The patient was started on fluids, a PPI, and transfused 2 units of pRBCs. Gastroenterology planned a colonoscopy the following day. Colonoscopy was notable for blood throughout the colon, a non-bleeding ulcer in the ascending colon with stigmata of recent bleeding, and a foreign body resembling a large fecalith (Figure 1/2). The fecalith appeared white after irrigation and was unable to be broken up via rat-tooth forceps. Repeat, imaging confirmed 4.9 cm barium fecalith. Repeat colonoscopy for barium break up and evacuation was unsuccessful due to persistent bleeding. Surgery was consulted. The patient would continue to experience hematochezia and required an additional unit of pRBC. At this time, surgery proceeded with a right hemicolectomy with removal of barium fecalith. Post op, the patient remained stable without transfusions.
Discussion: Gastrointestinal bleeds are significant and the approach for management is important. We present a unique case of hardened 4.9 cm barium fecalith causing bleeding ulceration in the ascending colon. As physicians, it is important to consider all outcomes when ordering a test, performing a procedure, or prescribing a treatment. We aimed to raise awareness that performing a simple test like a barium enema can even cause a bleed.

Figure: Both Figure 1 & 2 illustrate the large barium filled fecalith located in the cecum
Disclosures:
Shane Quo indicated no relevant financial relationships.
Mary Parianos indicated no relevant financial relationships.
Alyssa Benjamin indicated no relevant financial relationships.
Charles Hotte indicated no relevant financial relationships.
Shane Quo, DO1, Mary Parianos, MD2, Alyssa Benjamin, DO1, Charles Hotte, MD3. P3479 - Unique Case of Bleeding Barium Contrast Fecalith, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
