Tuesday Poster Session
Category: GI Bleeding
P3482 - Ischemic Gastritis Secondary to Aortic Dissection
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Duha Zaffar, MBBS, MD
University of Maryland Medical Center Midtown Campus
Baltimore, MD
Presenting Author(s)
Duha Zaffar, MBBS, MD1, Stephen Schwartz, DO2, Osman Ali, MD3, Lauren George, MD3
1University of Maryland Medical Center Midtown Campus, Baltimore, MD; 2University of Maryland Medical System, Baltimore, MD; 3University of Maryland School of Medicine, Baltimore, MD
Introduction: Ischemic gastritis is rare, given that blood supply of stomach is rich. It is associated with a high mortality; therefore, early recognition is important for choosing appropriate course of management.The aim of this case report is to heighten awareness regarding the possibility of ischemic gastritis in the presence of conditions that can limit blood flow to stomach. We also discuss the role of hemostatic spray in controlling active bleeding in this scenario.
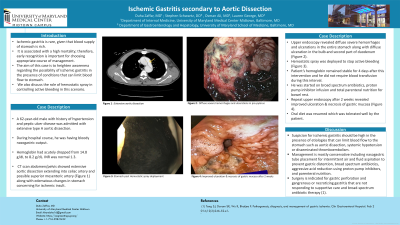
Case Description/Methods: A 62-year-old male with history of hypertension and peptic ulcer disease was admitted with extensive type A aortic dissection. During hospital course, he was having bloody nasogastric output. Hemoglobin had acutely dropped from 14.8 g/dL to 8.2 g/dL. INR was normal 1.3. CT scan abdomen/pelvis showed extensive aortic dissection extending into celiac artery and possible superior mesenteric artery (Figure 1) along with edematous changes in stomach concerning for ischemic insult. Upper endoscopy revealed diffuse severe hemorrhages and ulcerations in the entire stomach along with diffuse ulceration in the bulb and second part of duodenum (Figure 2). Hemostatic spray was deployed to stop active bleeding (Figure 3). Patient’s hemoglobin remained stable for 4 days after this intervention and he did not require blood transfusion during this interval. He was started on broad spectrum antibiotics, proton pump inhibitor infusion and total parenteral nutrition for bowel rest. Repeat upper endoscopy after 2 weeks revealed improved ulceration & necrosis of gastric mucosa (Figure 4). Oral diet was resumed which was tolerated well by the patient.
Discussion: Suspicion for ischemic gastritis should be high in the presence of etiologies that can limit blood flow to the stomach such as aortic dissection, systemic hypotension or disseminated thromboembolism. Management is mostly conservative including nasogastric tube placement for intermittent air and fluid aspiration to prevent gastric distention, broad spectrum antibiotics, aggressive acid reduction using proton pump inhibitors, and parenteral nutrition. Surgery is indicated for gastric perforation and gangrenous or necrotizing gastritis that are not responding to supportive care and broad-spectrum antibiotic therapy (1). (1)Tang SJ, Daram SR, Wu R, Bhaijee F. Pathogenesis, diagnosis, and management of gastric ischemia. Clin Gastroenterol Hepatol. Feb 2014;12(2):246-52.e1.

Disclosures:
Duha Zaffar, MBBS, MD1, Stephen Schwartz, DO2, Osman Ali, MD3, Lauren George, MD3. P3482 - Ischemic Gastritis Secondary to Aortic Dissection, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Maryland Medical Center Midtown Campus, Baltimore, MD; 2University of Maryland Medical System, Baltimore, MD; 3University of Maryland School of Medicine, Baltimore, MD
Introduction: Ischemic gastritis is rare, given that blood supply of stomach is rich. It is associated with a high mortality; therefore, early recognition is important for choosing appropriate course of management.The aim of this case report is to heighten awareness regarding the possibility of ischemic gastritis in the presence of conditions that can limit blood flow to stomach. We also discuss the role of hemostatic spray in controlling active bleeding in this scenario.
Case Description/Methods: A 62-year-old male with history of hypertension and peptic ulcer disease was admitted with extensive type A aortic dissection. During hospital course, he was having bloody nasogastric output. Hemoglobin had acutely dropped from 14.8 g/dL to 8.2 g/dL. INR was normal 1.3. CT scan abdomen/pelvis showed extensive aortic dissection extending into celiac artery and possible superior mesenteric artery (Figure 1) along with edematous changes in stomach concerning for ischemic insult. Upper endoscopy revealed diffuse severe hemorrhages and ulcerations in the entire stomach along with diffuse ulceration in the bulb and second part of duodenum (Figure 2). Hemostatic spray was deployed to stop active bleeding (Figure 3). Patient’s hemoglobin remained stable for 4 days after this intervention and he did not require blood transfusion during this interval. He was started on broad spectrum antibiotics, proton pump inhibitor infusion and total parenteral nutrition for bowel rest. Repeat upper endoscopy after 2 weeks revealed improved ulceration & necrosis of gastric mucosa (Figure 4). Oral diet was resumed which was tolerated well by the patient.
Discussion: Suspicion for ischemic gastritis should be high in the presence of etiologies that can limit blood flow to the stomach such as aortic dissection, systemic hypotension or disseminated thromboembolism. Management is mostly conservative including nasogastric tube placement for intermittent air and fluid aspiration to prevent gastric distention, broad spectrum antibiotics, aggressive acid reduction using proton pump inhibitors, and parenteral nutrition. Surgery is indicated for gastric perforation and gangrenous or necrotizing gastritis that are not responding to supportive care and broad-spectrum antibiotic therapy (1). (1)Tang SJ, Daram SR, Wu R, Bhaijee F. Pathogenesis, diagnosis, and management of gastric ischemia. Clin Gastroenterol Hepatol. Feb 2014;12(2):246-52.e1.

Figure: 1: Extensive aortic dissection
2: Diffuse severe hemorrhages and ulcerations in pre-pylorus
3: Stomach post Hemostatic spray deployment
4: Improved ulceration & necrosis of gastric mucosa after 2 weeks
2: Diffuse severe hemorrhages and ulcerations in pre-pylorus
3: Stomach post Hemostatic spray deployment
4: Improved ulceration & necrosis of gastric mucosa after 2 weeks
Disclosures:
Duha Zaffar indicated no relevant financial relationships.
Stephen Schwartz indicated no relevant financial relationships.
Osman Ali indicated no relevant financial relationships.
Lauren George indicated no relevant financial relationships.
Duha Zaffar, MBBS, MD1, Stephen Schwartz, DO2, Osman Ali, MD3, Lauren George, MD3. P3482 - Ischemic Gastritis Secondary to Aortic Dissection, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
