Tuesday Poster Session
Category: GI Bleeding
P3483 - A Soccer Game Turned Bloody: A Case of Ischemic Colitis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Duha Zaffar, MBBS, MD
University of Maryland Medical Center Midtown Campus
Baltimore, MD
Presenting Author(s)
Duha Zaffar, MBBS, MD1, Stephen Schwartz, DO2, Osman Ali, MD3, Bruce D. Greenwald, MD3
1University of Maryland Medical Center Midtown Campus, Baltimore, MD; 2University of Maryland Medical System, Baltimore, MD; 3University of Maryland School of Medicine, Baltimore, MD
Introduction: Ischemic colitis in young adults is rare. The incidence in adults less than 40 years is 1.1 per 100,000. It can present with abdominal pain and rectal bleeding after vigorous exercise. In one study, 2% of marathon runners reported blood in stool following races, and 20% of runners had positive fecal occult blood test (FOBT) after marathons (1). The aim of this case report is to heighten awareness of ischemic colitis as possible cause for gastrointestinal bleed in those with recent sports activity.
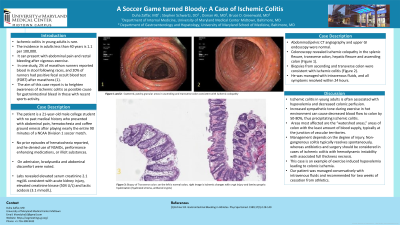
Case Description/Methods: The patient is a 21-year-old male college student with no past medical history who presented with abdominal pain, hematochezia and coffee ground emesis after playing nearly the entire 90 minutes of a NCAA Division 1 soccer match. No prior episodes of hematochezia reported, and he denied use of NSAIDs, performance enhancing medications, or illicit substances. On admission, bradycardia and abdominal discomfort were noted. Labs revealed elevated serum creatinine 2.1 mg/dL consistent with acute kidney injury, elevated creatinine kinase (504 U/L) and lactic acidosis (3.1 mmol/L). Abdominal/pelvic CT angiography and upper GI endoscopy were normal. Colonoscopy revealed ischemic colopathy in the splenic flexure, transverse colon, hepatic flexure and ascending colon (Figure 1). Biopsies from ascending and transverse colon were consistent with ischemic colitis (Figure 2). He was managed with intravenous fluids, and all symptoms resolved within 24 hours.
Discussion: Ischemic colitis in young adults is often associated with hypovolemia and decreased colonic perfusion. Increased sympathetic tone during exercise in hot environment can cause decreased blood flow to colon by 50-80%, thus precipitating ischemic colitis. Areas most affected are the “watershed areas,” areas of colon with the least amount of blood supply, typically at the junction of vascular territories. Management depends on the degree of injury. Non-gangrenous colitis typically resolves spontaneously, whereas antibiotics and surgery should be considered in cases of ischemic colitis with hemodynamic instability with associated full thickness necrosis. This case is an example of exercise induced hypovolemia leading to colonic ischemia. Our patient was managed conservatively with intravenous fluids and recommended for two weeks of cessation from athletics.
(1)Eichner ER. Gastrointestinal Bleeding in Athletes. Phys Sportsmed. 1989;17(5):128-140

Disclosures:
Duha Zaffar, MBBS, MD1, Stephen Schwartz, DO2, Osman Ali, MD3, Bruce D. Greenwald, MD3. P3483 - A Soccer Game Turned Bloody: A Case of Ischemic Colitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Maryland Medical Center Midtown Campus, Baltimore, MD; 2University of Maryland Medical System, Baltimore, MD; 3University of Maryland School of Medicine, Baltimore, MD
Introduction: Ischemic colitis in young adults is rare. The incidence in adults less than 40 years is 1.1 per 100,000. It can present with abdominal pain and rectal bleeding after vigorous exercise. In one study, 2% of marathon runners reported blood in stool following races, and 20% of runners had positive fecal occult blood test (FOBT) after marathons (1). The aim of this case report is to heighten awareness of ischemic colitis as possible cause for gastrointestinal bleed in those with recent sports activity.
Case Description/Methods: The patient is a 21-year-old male college student with no past medical history who presented with abdominal pain, hematochezia and coffee ground emesis after playing nearly the entire 90 minutes of a NCAA Division 1 soccer match. No prior episodes of hematochezia reported, and he denied use of NSAIDs, performance enhancing medications, or illicit substances. On admission, bradycardia and abdominal discomfort were noted. Labs revealed elevated serum creatinine 2.1 mg/dL consistent with acute kidney injury, elevated creatinine kinase (504 U/L) and lactic acidosis (3.1 mmol/L). Abdominal/pelvic CT angiography and upper GI endoscopy were normal. Colonoscopy revealed ischemic colopathy in the splenic flexure, transverse colon, hepatic flexure and ascending colon (Figure 1). Biopsies from ascending and transverse colon were consistent with ischemic colitis (Figure 2). He was managed with intravenous fluids, and all symptoms resolved within 24 hours.
Discussion: Ischemic colitis in young adults is often associated with hypovolemia and decreased colonic perfusion. Increased sympathetic tone during exercise in hot environment can cause decreased blood flow to colon by 50-80%, thus precipitating ischemic colitis. Areas most affected are the “watershed areas,” areas of colon with the least amount of blood supply, typically at the junction of vascular territories. Management depends on the degree of injury. Non-gangrenous colitis typically resolves spontaneously, whereas antibiotics and surgery should be considered in cases of ischemic colitis with hemodynamic instability with associated full thickness necrosis. This case is an example of exercise induced hypovolemia leading to colonic ischemia. Our patient was managed conservatively with intravenous fluids and recommended for two weeks of cessation from athletics.
(1)Eichner ER. Gastrointestinal Bleeding in Athletes. Phys Sportsmed. 1989;17(5):128-140

Figure: Figure 1 and 2: Scattered and patchy granular areas in ascending and transverse colon consistent with ischemic colopathy
Figure 3: Colonic mucosa with focal ischemic changes
Figure 3: Colonic mucosa with focal ischemic changes
Disclosures:
Duha Zaffar indicated no relevant financial relationships.
Stephen Schwartz indicated no relevant financial relationships.
Osman Ali indicated no relevant financial relationships.
Bruce Greenwald: Steris Endoscopy – Consultant, Grant/Research Support.
Duha Zaffar, MBBS, MD1, Stephen Schwartz, DO2, Osman Ali, MD3, Bruce D. Greenwald, MD3. P3483 - A Soccer Game Turned Bloody: A Case of Ischemic Colitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
