Tuesday Poster Session
Category: GI Bleeding
P3486 - Hemosuccus Pancreaticus: A Rare Cause of Upper GI Bleeding
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Adam Z. Koller, DO, MS
Palmetto General Hospital
Coral Gables, FL
Presenting Author(s)
Adam Z. Koller, DO, MS1, Aamir Pervez, DO2, Roselys Ibanez, MD2, Melissa Matheus, MD3, Karthik Mohan, DO4, IIan Rzadkowolsky-Raoli, MD2
1Palmetto General Hospital, Coral Gables, FL; 2Palmetto General Hospital, Hialeah, FL; 3Larkin Community Hospital, Palm Springs Campus, Doral, FL; 4Larkin Community Hospital, Miami, FL
Introduction: Hemosuccus pancreaticus (HP) is a rare cause of upper gastrointestinal bleeding (GIB) which can be fatal if not recognized in a timely manner. We present a case of HP in a young male in which angiographic intervention was lifesaving.
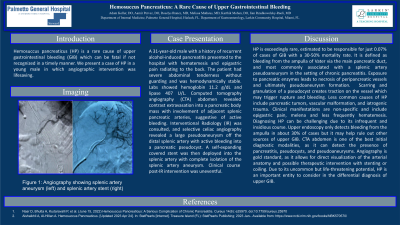
Case Description/Methods: A 31-year-old male with a history of recurrent alcohol-induced pancreatitis presented to the hospital with hematemesis and epigastric pain radiating to the back. The patient had severe abdominal tenderness without guarding and was hemodynamically stable. Labs showed hemoglobin 11.2 g/dL and lipase 407 U/L. Computed tomography angiography (CTA) abdomen revealed contrast extravasation into a pancreatic body mass with involvement of adjacent splenic pancreatic arteries, suggestive of active bleeding. Interventional Radiology (IR) was consulted, and selective celiac angiography revealed a large pseudoaneurysm off the distal splenic artery with active bleeding into a pancreatic pseudocyst. A self-expanding covered stent was then deployed into the splenic artery with complete isolation of the splenic artery aneurysm. Clinical course post-IR intervention was uneventful.
Discussion: HP is exceedingly rare, estimated to be responsible for just 0.07% of cases of GIB with a 30-50% mortality rate. It is defined as bleeding from the ampulla of Vater via the main pancreatic duct, and most commonly associated with a splenic artery pseudoaneurysm in the setting of chronic pancreatitis. Exposure to pancreatic enzymes leads to necrosis of peripancreatic vessels and ultimately pseudoaneurysm formation. Scarring and granulation of a pseudocyst creates traction on the vessel which may trigger rupture and bleeding. Less common causes of HP include pancreatic tumors, vascular malformation, and iatrogenic trauma. Clinical manifestations are non-specific and include epigastric pain, melena and less frequently hematemesis. Diagnosing HP can be challenging due to its infrequent and insidious course. Upper endoscopy only detects bleeding from the ampulla in about 30% of cases but it may help rule out other sources of upper GIB. CTA abdomen is one of the best initial diagnostic modalities, as it can detect the presence of pancreatitis, pseudocysts, and pseudoaneurysms. Angiography is gold standard, as it allows for direct visualization of the arterial anatomy and possible therapeutic intervention with stenting or coiling. Due to its uncommon but life-threatening potential, HP is an important entity to consider in the differential diagnosis of upper GIB.

Disclosures:
Adam Z. Koller, DO, MS1, Aamir Pervez, DO2, Roselys Ibanez, MD2, Melissa Matheus, MD3, Karthik Mohan, DO4, IIan Rzadkowolsky-Raoli, MD2. P3486 - Hemosuccus Pancreaticus: A Rare Cause of Upper GI Bleeding, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Palmetto General Hospital, Coral Gables, FL; 2Palmetto General Hospital, Hialeah, FL; 3Larkin Community Hospital, Palm Springs Campus, Doral, FL; 4Larkin Community Hospital, Miami, FL
Introduction: Hemosuccus pancreaticus (HP) is a rare cause of upper gastrointestinal bleeding (GIB) which can be fatal if not recognized in a timely manner. We present a case of HP in a young male in which angiographic intervention was lifesaving.
Case Description/Methods: A 31-year-old male with a history of recurrent alcohol-induced pancreatitis presented to the hospital with hematemesis and epigastric pain radiating to the back. The patient had severe abdominal tenderness without guarding and was hemodynamically stable. Labs showed hemoglobin 11.2 g/dL and lipase 407 U/L. Computed tomography angiography (CTA) abdomen revealed contrast extravasation into a pancreatic body mass with involvement of adjacent splenic pancreatic arteries, suggestive of active bleeding. Interventional Radiology (IR) was consulted, and selective celiac angiography revealed a large pseudoaneurysm off the distal splenic artery with active bleeding into a pancreatic pseudocyst. A self-expanding covered stent was then deployed into the splenic artery with complete isolation of the splenic artery aneurysm. Clinical course post-IR intervention was uneventful.
Discussion: HP is exceedingly rare, estimated to be responsible for just 0.07% of cases of GIB with a 30-50% mortality rate. It is defined as bleeding from the ampulla of Vater via the main pancreatic duct, and most commonly associated with a splenic artery pseudoaneurysm in the setting of chronic pancreatitis. Exposure to pancreatic enzymes leads to necrosis of peripancreatic vessels and ultimately pseudoaneurysm formation. Scarring and granulation of a pseudocyst creates traction on the vessel which may trigger rupture and bleeding. Less common causes of HP include pancreatic tumors, vascular malformation, and iatrogenic trauma. Clinical manifestations are non-specific and include epigastric pain, melena and less frequently hematemesis. Diagnosing HP can be challenging due to its infrequent and insidious course. Upper endoscopy only detects bleeding from the ampulla in about 30% of cases but it may help rule out other sources of upper GIB. CTA abdomen is one of the best initial diagnostic modalities, as it can detect the presence of pancreatitis, pseudocysts, and pseudoaneurysms. Angiography is gold standard, as it allows for direct visualization of the arterial anatomy and possible therapeutic intervention with stenting or coiling. Due to its uncommon but life-threatening potential, HP is an important entity to consider in the differential diagnosis of upper GIB.

Figure: (A) Angiography showing splenic artery aneurysm (B) splenic artery stent
Disclosures:
Adam Koller indicated no relevant financial relationships.
Aamir Pervez indicated no relevant financial relationships.
Roselys Ibanez indicated no relevant financial relationships.
Melissa Matheus indicated no relevant financial relationships.
Karthik Mohan indicated no relevant financial relationships.
IIan Rzadkowolsky-Raoli indicated no relevant financial relationships.
Adam Z. Koller, DO, MS1, Aamir Pervez, DO2, Roselys Ibanez, MD2, Melissa Matheus, MD3, Karthik Mohan, DO4, IIan Rzadkowolsky-Raoli, MD2. P3486 - Hemosuccus Pancreaticus: A Rare Cause of Upper GI Bleeding, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
