Tuesday Poster Session
Category: GI Bleeding
P3487 - Upper Gastrointestinal Bleed as First Presentation of Duodenal Mucosal Melanoma
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Mark Rigby, DO
Ascension Genesys Hospital
Grand Blanc, MI
Presenting Author(s)
Mark Rigby, DO, Brandon Wiggins, DO, MPH, Kyle Knight, DO, Fady Banno, MD, MS, Jacob Burch, DO, Justin Miller, DO
Ascension Genesys Hospital, Grand Blanc, MI
Introduction: Melanoma is the fifth most common malignancy in the United States with intestinal metastases often found on autopsy. Here we present a case of a symptomatic duodenal lesion as the first presentation of melanoma, without cutaneous manifestation.
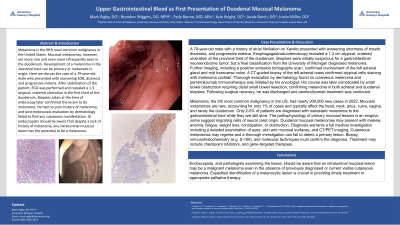
Case Description/Methods: A 79-year-old male with a history of atrial fibrillation on Xarelto presented with worsening shortness of breath, dizziness, and progressive melena. Esophagogastroduodenoscopy revealed a 1.3 cm atypical, cratered ulceration at the proximal third of the duodenum. Biopsies were initially suspicious for a gastrointestinal neuroendocrine tumor, but a final classification from the University of Michigan diagnosed melanoma. Further imaging, including a positron emission tomography scan, confirmed involvement of the left adrenal gland and mid transverse colon. A CT-guided biopsy of the left adrenal mass confirmed atypical cells staining with melanoma cocktail. Thorough evaluation by dermatology found no cutaneous melanoma and pembrolizumab immunotherapy was initiated by his oncologist. His course was later complicated by small bowel obstruction requiring distal small bowel resection, confirming melanoma in both adrenal and duodenal biopsies. Following surgical recovery, he was discharged and pembrolizumab treatment was continued.
Discussion: Melanoma, the fifth most common malignancy in the US, had nearly 200,000 new cases in 2022. Mucosal melanomas are rare, accounting for only 1% of cases and typically affect the head, neck, anus, vulva, vagina, and rarely the duodenum. Only 2-5% of patients are diagnosed with metastatic melanoma to the gastrointestinal tract while they are still alive. The pathophysiology of primary mucosal lesions is an enigma, some suggest migrating cells of neural crest origin. Duodenal mucosal melanomas may present with melena, anemia, fatigue, weight loss, constipation, or obstruction. Diagnosis warrants a full medical investigation including a detailed examination of eyes, skin and mucosal surfaces, and CT/PET imaging. Cutaneous melanomas may regress and a thorough investigation can fail to detect a primary lesion. Biopsy, immunohistochemistry (e.g. S-100), and molecular techniques must confirm the diagnosis. Treatment may include checkpoint inhibitors, and gene-targeted therapies. Endoscopists should be aware that an intraluminal mucosal lesion may be malignant melanoma even in the absence of previously diagnosed or visible cutaneous melanoma.

Disclosures:
Mark Rigby, DO, Brandon Wiggins, DO, MPH, Kyle Knight, DO, Fady Banno, MD, MS, Jacob Burch, DO, Justin Miller, DO. P3487 - Upper Gastrointestinal Bleed as First Presentation of Duodenal Mucosal Melanoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Ascension Genesys Hospital, Grand Blanc, MI
Introduction: Melanoma is the fifth most common malignancy in the United States with intestinal metastases often found on autopsy. Here we present a case of a symptomatic duodenal lesion as the first presentation of melanoma, without cutaneous manifestation.
Case Description/Methods: A 79-year-old male with a history of atrial fibrillation on Xarelto presented with worsening shortness of breath, dizziness, and progressive melena. Esophagogastroduodenoscopy revealed a 1.3 cm atypical, cratered ulceration at the proximal third of the duodenum. Biopsies were initially suspicious for a gastrointestinal neuroendocrine tumor, but a final classification from the University of Michigan diagnosed melanoma. Further imaging, including a positron emission tomography scan, confirmed involvement of the left adrenal gland and mid transverse colon. A CT-guided biopsy of the left adrenal mass confirmed atypical cells staining with melanoma cocktail. Thorough evaluation by dermatology found no cutaneous melanoma and pembrolizumab immunotherapy was initiated by his oncologist. His course was later complicated by small bowel obstruction requiring distal small bowel resection, confirming melanoma in both adrenal and duodenal biopsies. Following surgical recovery, he was discharged and pembrolizumab treatment was continued.
Discussion: Melanoma, the fifth most common malignancy in the US, had nearly 200,000 new cases in 2022. Mucosal melanomas are rare, accounting for only 1% of cases and typically affect the head, neck, anus, vulva, vagina, and rarely the duodenum. Only 2-5% of patients are diagnosed with metastatic melanoma to the gastrointestinal tract while they are still alive. The pathophysiology of primary mucosal lesions is an enigma, some suggest migrating cells of neural crest origin. Duodenal mucosal melanomas may present with melena, anemia, fatigue, weight loss, constipation, or obstruction. Diagnosis warrants a full medical investigation including a detailed examination of eyes, skin and mucosal surfaces, and CT/PET imaging. Cutaneous melanomas may regress and a thorough investigation can fail to detect a primary lesion. Biopsy, immunohistochemistry (e.g. S-100), and molecular techniques must confirm the diagnosis. Treatment may include checkpoint inhibitors, and gene-targeted therapies. Endoscopists should be aware that an intraluminal mucosal lesion may be malignant melanoma even in the absence of previously diagnosed or visible cutaneous melanoma.

Figure: A) 1.3 cm atypical, ulcerated lesion seen at the proximal third of the duodenum. B) Follow-up outpatient endoscopy of same lesion. C) 400 power H&E stain (only tumor cells displayed). D) S-100 immunostain at 20x
Disclosures:
Mark Rigby indicated no relevant financial relationships.
Brandon Wiggins indicated no relevant financial relationships.
Kyle Knight indicated no relevant financial relationships.
Fady Banno indicated no relevant financial relationships.
Jacob Burch indicated no relevant financial relationships.
Justin Miller indicated no relevant financial relationships.
Mark Rigby, DO, Brandon Wiggins, DO, MPH, Kyle Knight, DO, Fady Banno, MD, MS, Jacob Burch, DO, Justin Miller, DO. P3487 - Upper Gastrointestinal Bleed as First Presentation of Duodenal Mucosal Melanoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
