Tuesday Poster Session
Category: GI Bleeding
P3491 - Stiff Person Syndrome Presenting with Ischemic Colitis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
Benjamin Heriford, DO
UT Health San Antonio
San Antonio, TX
Presenting Author(s)
Benjamin Heriford, DO1, Lily Kuo, MD2, Hamza Khan, MD1, Jonathan Selzman, DO3, Kendra Stillwell, DO4, Chandraprakash Umapathy, MD, MS3
1UT Health San Antonio, San Antonio, TX; 2University of Texas Health Science Center San Antonio, San Antonio, TX; 3University of Texas Health Science Center at San Antonio, San Antonio, TX; 4Brooke Army Medical Center, Fort Sam Houston, TX
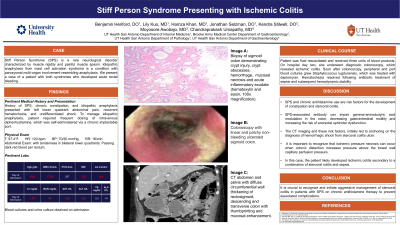
Introduction: Stiff Person Syndrome (SPS) is a rare neurological disorder characterized by muscle rigidity and painful muscle spasm associated with anti-glutamic acid decarboxylase antibody. Idiopathic anaphylaxis from mast cell activation syndrome is a condition with paroxysmal multi-organ involvement resembling anaphylaxis. We present a case of a patient with both syndromes who developed acute rectal bleeding.
Case Description/Methods: A 52-year-old female with a history of SPS, chronic constipation, and idiopathic anaphylaxis presented with one day of left lower quadrant abdominal pain, recurrent hematochezia, and undifferentiated shock. Of note, to manage her idiopathic anaphylaxis, she required frequent dosing of intravenous diphenhydramine, which she self-administered via a chronic implantable port. Initial vitals showed a blood pressure of 70/30 mmHg and heart rate at 120 BPM. Labs revealed rising lactic acid at 4.0 mmol/L. Patient was fluid resuscitated and received three units of blood products. CT imaging demonstrated a large stool burden and a dilated colon, concerning for stercoral colitis. On hospital day two, she underwent diagnostic colonoscopy, which revealed patchy, linear ulcerations in the rectosigmoid colon, endoscopically consistent with ischemic colitis. Soon after colonoscopy, peripheral and port blood cultures grew Staphylococcus lugdunensis, which was treated with daptomycin. Hematochezia resolved following antibiotic treatment of sepsis and subsequent hemodynamic stability.
Discussion: SPS and chronic antihistamine use are risk factors for the development of constipation and stercoral colitis. SPS-associated antibody can impair gamma-aminobutyric acid modulation in the colon, decreasing gastrointestinal motility and increasing the risk of anorectal sphincter dysfunction. The CT imaging and these risk factors, initially led to anchoring on the diagnosis of hemorrhagic shock from stercoral colitis ulcer. It is important to recognize that ischemic pressure necrosis can occur when colonic distention increases pressure above the bowel wall capillary perfusion pressure. In this case, the patient likely developed ischemic colitis secondary to a combination of stercoral colitis and sepsis. It is crucial to recognize and initiate aggressive management of stercoral colitis in patients with SPS on chronic antihistamine therapy to prevent associated complications.
Disclosures:
Benjamin Heriford, DO1, Lily Kuo, MD2, Hamza Khan, MD1, Jonathan Selzman, DO3, Kendra Stillwell, DO4, Chandraprakash Umapathy, MD, MS3. P3491 - Stiff Person Syndrome Presenting with Ischemic Colitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1UT Health San Antonio, San Antonio, TX; 2University of Texas Health Science Center San Antonio, San Antonio, TX; 3University of Texas Health Science Center at San Antonio, San Antonio, TX; 4Brooke Army Medical Center, Fort Sam Houston, TX
Introduction: Stiff Person Syndrome (SPS) is a rare neurological disorder characterized by muscle rigidity and painful muscle spasm associated with anti-glutamic acid decarboxylase antibody. Idiopathic anaphylaxis from mast cell activation syndrome is a condition with paroxysmal multi-organ involvement resembling anaphylaxis. We present a case of a patient with both syndromes who developed acute rectal bleeding.
Case Description/Methods: A 52-year-old female with a history of SPS, chronic constipation, and idiopathic anaphylaxis presented with one day of left lower quadrant abdominal pain, recurrent hematochezia, and undifferentiated shock. Of note, to manage her idiopathic anaphylaxis, she required frequent dosing of intravenous diphenhydramine, which she self-administered via a chronic implantable port. Initial vitals showed a blood pressure of 70/30 mmHg and heart rate at 120 BPM. Labs revealed rising lactic acid at 4.0 mmol/L. Patient was fluid resuscitated and received three units of blood products. CT imaging demonstrated a large stool burden and a dilated colon, concerning for stercoral colitis. On hospital day two, she underwent diagnostic colonoscopy, which revealed patchy, linear ulcerations in the rectosigmoid colon, endoscopically consistent with ischemic colitis. Soon after colonoscopy, peripheral and port blood cultures grew Staphylococcus lugdunensis, which was treated with daptomycin. Hematochezia resolved following antibiotic treatment of sepsis and subsequent hemodynamic stability.
Discussion: SPS and chronic antihistamine use are risk factors for the development of constipation and stercoral colitis. SPS-associated antibody can impair gamma-aminobutyric acid modulation in the colon, decreasing gastrointestinal motility and increasing the risk of anorectal sphincter dysfunction. The CT imaging and these risk factors, initially led to anchoring on the diagnosis of hemorrhagic shock from stercoral colitis ulcer. It is important to recognize that ischemic pressure necrosis can occur when colonic distention increases pressure above the bowel wall capillary perfusion pressure. In this case, the patient likely developed ischemic colitis secondary to a combination of stercoral colitis and sepsis. It is crucial to recognize and initiate aggressive management of stercoral colitis in patients with SPS on chronic antihistamine therapy to prevent associated complications.
Disclosures:
Benjamin Heriford indicated no relevant financial relationships.
Lily Kuo indicated no relevant financial relationships.
Hamza Khan indicated no relevant financial relationships.
Jonathan Selzman indicated no relevant financial relationships.
Kendra Stillwell indicated no relevant financial relationships.
Chandraprakash Umapathy indicated no relevant financial relationships.
Benjamin Heriford, DO1, Lily Kuo, MD2, Hamza Khan, MD1, Jonathan Selzman, DO3, Kendra Stillwell, DO4, Chandraprakash Umapathy, MD, MS3. P3491 - Stiff Person Syndrome Presenting with Ischemic Colitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
