Tuesday Poster Session
Category: GI Bleeding
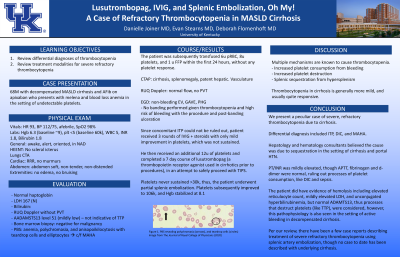
P3496 - Lusutrombopag, IVIG, and Splenic Embolization, Oh My! A Case of Refractory Thrombocytopenia in NASH Cirrhosis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- DJ
Danielle Joiner, MD
University of Kentucky
Lexington, KY
Presenting Author(s)
Danielle Joiner, MD, Evan Stearns, MD, Deborah Flomenhoft, MD
University of Kentucky, Lexington, KY
Introduction: Multiple mechanisms are known to cause thrombocytopenia. Increased platelet consumption from bleeding, increased platelet destruction, and splenic sequestration from hypersplenism are the most common pathophysiological processes causing thrombocytopenia. Thrombocytopenia in cirrhosis is generally more mild, and usually quite responsive. Here, we present a case of thrombocytopenia in a cirrhotic severely refractory to replacement and various therapy modalities.
Case Description/Methods: 68M with decompensated NASH cirrhosis and AFib on eliquis who presents with melena and blood loss anemia in setting of undetectable platelets. Patient was tachycardic, normotensive and afebrile. Labs were notable for Hgb 6 (baseline 9), plt < 5 (baseline ~60k). PBS revealed anemia, polychromasia & anisopoikilocytosis. Haptoglobin and LDH were normal. The patient was subsequently transfused 6u pRBC, 8u of platelets, and 1u FFP within the first 24 hours, without platelet response. CTAP revealed cirrhosis, splenomegaly and patent hepatic vasculature. Doppler revealed normal flow. EGD revealed non-bleeding EV, GAVE, and PHD. Since concomitant ITP could not be ruled out, patient received IVIG + steroids with only mild, non-sustained improvement. He received an additional 12u platelets, and completed a course of lusutrombopag, a thrombopoietin receptor agonist used in cirrhotics prior to procedures, in an attempt to safely proceed with TIPS. Platelets never sustained >30k, thus partial splenic embolization was performed and platelets improved to 106k and hemoglobin stabilized at 8.1.
Discussion: We present a peculiar case of severe, refractory thrombocytopenia due to cirrhosis. Differential diagnosis included ITP, DIC, and MAHA. Hepatology and hematology consultants believed the cause was due to sequestration from splenomegaly and cirrhosis. PT/INR was mildly elevated, though APTT, fibrinogen and d-dimer were normal, ruling out processes of platelet consumption, like DIC and sepsis. The patient did have evidence of hemolysis including elevated reticulocyte count, mildly elevated LDH, and unconjugated hyperbilirubinemia, but normal ADAMTS13, thus processes that destruct platelets (like TTP), were considered, however this pathophysiology is also seen in the setting of active bleeding in decompensated cirrhosis. Per our review, there have been a few case reports describing treatment of severe refractory thrombocytopenia using splenic artery embolization, though no case to date has been described with underlying cirrhosis.
Disclosures:
Danielle Joiner, MD, Evan Stearns, MD, Deborah Flomenhoft, MD. P3496 - Lusutrombopag, IVIG, and Splenic Embolization, Oh My! A Case of Refractory Thrombocytopenia in NASH Cirrhosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Kentucky, Lexington, KY
Introduction: Multiple mechanisms are known to cause thrombocytopenia. Increased platelet consumption from bleeding, increased platelet destruction, and splenic sequestration from hypersplenism are the most common pathophysiological processes causing thrombocytopenia. Thrombocytopenia in cirrhosis is generally more mild, and usually quite responsive. Here, we present a case of thrombocytopenia in a cirrhotic severely refractory to replacement and various therapy modalities.
Case Description/Methods: 68M with decompensated NASH cirrhosis and AFib on eliquis who presents with melena and blood loss anemia in setting of undetectable platelets. Patient was tachycardic, normotensive and afebrile. Labs were notable for Hgb 6 (baseline 9), plt < 5 (baseline ~60k). PBS revealed anemia, polychromasia & anisopoikilocytosis. Haptoglobin and LDH were normal. The patient was subsequently transfused 6u pRBC, 8u of platelets, and 1u FFP within the first 24 hours, without platelet response. CTAP revealed cirrhosis, splenomegaly and patent hepatic vasculature. Doppler revealed normal flow. EGD revealed non-bleeding EV, GAVE, and PHD. Since concomitant ITP could not be ruled out, patient received IVIG + steroids with only mild, non-sustained improvement. He received an additional 12u platelets, and completed a course of lusutrombopag, a thrombopoietin receptor agonist used in cirrhotics prior to procedures, in an attempt to safely proceed with TIPS. Platelets never sustained >30k, thus partial splenic embolization was performed and platelets improved to 106k and hemoglobin stabilized at 8.1.
Discussion: We present a peculiar case of severe, refractory thrombocytopenia due to cirrhosis. Differential diagnosis included ITP, DIC, and MAHA. Hepatology and hematology consultants believed the cause was due to sequestration from splenomegaly and cirrhosis. PT/INR was mildly elevated, though APTT, fibrinogen and d-dimer were normal, ruling out processes of platelet consumption, like DIC and sepsis. The patient did have evidence of hemolysis including elevated reticulocyte count, mildly elevated LDH, and unconjugated hyperbilirubinemia, but normal ADAMTS13, thus processes that destruct platelets (like TTP), were considered, however this pathophysiology is also seen in the setting of active bleeding in decompensated cirrhosis. Per our review, there have been a few case reports describing treatment of severe refractory thrombocytopenia using splenic artery embolization, though no case to date has been described with underlying cirrhosis.
Disclosures:
Danielle Joiner indicated no relevant financial relationships.
Evan Stearns indicated no relevant financial relationships.
Deborah Flomenhoft indicated no relevant financial relationships.
Danielle Joiner, MD, Evan Stearns, MD, Deborah Flomenhoft, MD. P3496 - Lusutrombopag, IVIG, and Splenic Embolization, Oh My! A Case of Refractory Thrombocytopenia in NASH Cirrhosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
