Tuesday Poster Session
Category: GI Bleeding
P3522 - Left Gastric Artery Pseudoaneurysm Resulting From Gastric Ulcer Presenting With Gastrointestinal Bleed
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- XL
Xue Jing Li, MD
University of Arizona College of Medicine
Phoenix, AZ
Presenting Author(s)
Xue Jing Li, MD, Sakolwan Suchartlikitwong, MD
University of Arizona College of Medicine, Phoenix, AZ
Introduction: Left gastric artery pseudoaneurysm (LGAP) is extremely rare and has been primarily associated with chronic pancreatitis or trauma. To date, there are only 2 case reports of penetrating gastric ulcer causing LGAP. Here, we report a patient with asymptomatic infrarenal aortic aneurysm (AA) who presented for hematemesis and was found to have a gastric ulcer eroding into a LGAP, treated with embolization.
Case Description/Methods: A 73 years-old male with obesity, hypertension, smoker presented for hematemesis. On arrival, he was hypotensive and required norepinephrine. Physical exam revealed soft abdomen and no tenderness. Laboratory test noted hemoglobin of 8.6 g/dL, elevated lactate to 2.8 mmol/L, AST 556/ALT 759 U/L, acute kidney injury with BUN 87 mg/dL, creatinine 3.73 mg/dL. A CTA abdomen/pelvis showed an infrarenal AA measuring 9.1cm (length) x 8.7cm (width) ending at the iliac bifurcation, fusiform enlargement of ascending aorta measuring 3.9cm, also contrast within the lumen of the stomach arising from the posterior lateral gastric wall consistent with active bleeding. He was intubated for airway support. Vascular surgery requested endoscopic evaluation for concern of primary aortoenteric fistula prior to endovascular repair.
On esophagogastroduodenoscopy, he was found to have a 4 cm oozing cratered lesion concerning for gastric ulcer at the incisura with large visible vessel. There was pulsation underneath the ulcer. Endoscopic ultrasound was attempted to evaluate for underlying blood vessel with limited visualization. Two hemostatic clips were placed for location marking. He was then taken down to interventional radiology, where angiogram demonstrated a visible 5mm LGA pseudoaneurysm corresponding to the visible vessel within the ulcer. NBCA/lipiodol glue embolization was performed successfully.
Patient then underwent percutaneous endovascular repair. He was scheduled for repeat endoscopy but was lost to follow-up.
Discussion: Visceral artery pseudoaneurysm are abnormal dilation, usually degenerative from loss of elastic fibers and reduced smooth muscle in tunica media. Causes include atherosclerosis, collagen disorder, trauma, infection, vasculitis, and pancreatitis. To date, there are 9 cases of splenic artery pseudoaneurysm and only 2 case of LGAP caused by peptic ulcer. In this patient who was already predisposed to collagen remodeling, we suspect that the ulcer eroded posteriorly and peptic enzymes contacted the vessel wall, compromising the vessel wall integrity leading to LGAP.

Disclosures:
Xue Jing Li, MD, Sakolwan Suchartlikitwong, MD. P3522 - Left Gastric Artery Pseudoaneurysm Resulting From Gastric Ulcer Presenting With Gastrointestinal Bleed, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Arizona College of Medicine, Phoenix, AZ
Introduction: Left gastric artery pseudoaneurysm (LGAP) is extremely rare and has been primarily associated with chronic pancreatitis or trauma. To date, there are only 2 case reports of penetrating gastric ulcer causing LGAP. Here, we report a patient with asymptomatic infrarenal aortic aneurysm (AA) who presented for hematemesis and was found to have a gastric ulcer eroding into a LGAP, treated with embolization.
Case Description/Methods: A 73 years-old male with obesity, hypertension, smoker presented for hematemesis. On arrival, he was hypotensive and required norepinephrine. Physical exam revealed soft abdomen and no tenderness. Laboratory test noted hemoglobin of 8.6 g/dL, elevated lactate to 2.8 mmol/L, AST 556/ALT 759 U/L, acute kidney injury with BUN 87 mg/dL, creatinine 3.73 mg/dL. A CTA abdomen/pelvis showed an infrarenal AA measuring 9.1cm (length) x 8.7cm (width) ending at the iliac bifurcation, fusiform enlargement of ascending aorta measuring 3.9cm, also contrast within the lumen of the stomach arising from the posterior lateral gastric wall consistent with active bleeding. He was intubated for airway support. Vascular surgery requested endoscopic evaluation for concern of primary aortoenteric fistula prior to endovascular repair.
On esophagogastroduodenoscopy, he was found to have a 4 cm oozing cratered lesion concerning for gastric ulcer at the incisura with large visible vessel. There was pulsation underneath the ulcer. Endoscopic ultrasound was attempted to evaluate for underlying blood vessel with limited visualization. Two hemostatic clips were placed for location marking. He was then taken down to interventional radiology, where angiogram demonstrated a visible 5mm LGA pseudoaneurysm corresponding to the visible vessel within the ulcer. NBCA/lipiodol glue embolization was performed successfully.
Patient then underwent percutaneous endovascular repair. He was scheduled for repeat endoscopy but was lost to follow-up.
Discussion: Visceral artery pseudoaneurysm are abnormal dilation, usually degenerative from loss of elastic fibers and reduced smooth muscle in tunica media. Causes include atherosclerosis, collagen disorder, trauma, infection, vasculitis, and pancreatitis. To date, there are 9 cases of splenic artery pseudoaneurysm and only 2 case of LGAP caused by peptic ulcer. In this patient who was already predisposed to collagen remodeling, we suspect that the ulcer eroded posteriorly and peptic enzymes contacted the vessel wall, compromising the vessel wall integrity leading to LGAP.

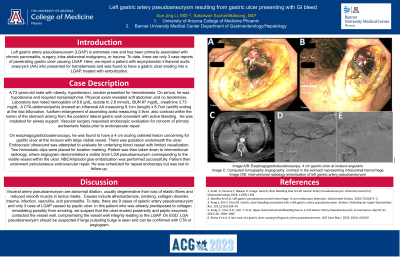
Figure: Image A/B: Esophagogastroduodenoscopy: 4 cm gastric ulcer at incisura angularis. Image C: Computed tomography angiography: contrast in the stomach representing intraluminal hemorrhage. Image D/E: Interventional radiology embolization of left gastric artery pseudoaneurysm
Disclosures:
Xue Jing Li indicated no relevant financial relationships.
Sakolwan Suchartlikitwong indicated no relevant financial relationships.
Xue Jing Li, MD, Sakolwan Suchartlikitwong, MD. P3522 - Left Gastric Artery Pseudoaneurysm Resulting From Gastric Ulcer Presenting With Gastrointestinal Bleed, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
