Tuesday Poster Session
Category: IBD
P3528 - Oral Vancomycin Is Associated With Less IBD Therapy Intensification in PSC-IBD
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Sarah M. Talamantes, MD
Stanford University
Mountain View, CA
Presenting Author(s)
Sarah M. Talamantes, MD1, Chiraag Kulkarni, MD2, George Cholankeril, MD3, Touran Fardeen, BS2, Sidhartha Sinha, MD2
1Stanford University, Mountain View, CA; 2Stanford University, Palo Alto, CA; 3Baylor University, Houston, TX
Introduction: Primary sclerosing cholangitis (PSC) is a progressive, cholestatic liver disease. About 70% of patients with PSC have co-morbid inflammatory bowel disease (IBD), typically ulcerative colitis (UC). There is no proven disease-modifying therapy for PSC, though oral vancomycin therapy (OVT) has received considerable interest. Anecdotally, patients with PSC-IBD treated with OVT seemed to have fewer IBD flares. To date, only case reports and a small case series have been published. We aim to determine the impact of OVT on IBD disease activity, estimated by therapy intensification, in patients with concomitant IBD and PSC.
Methods: This was a two-center, retrospective, self-controlled, cohort study. The study population included patients >18 years of age, confirmed diagnosis of PSC and IBD, history of OVT prescribed for the treatment of PSC after their diagnosis of IBD. Time off OVT was defined as any period after IBD diagnosis when the patient was not taking OVT. Therapy intensification was defined as therapy change, dose escalation or steroid prescription. Patients served as their own control, comparing number of therapy intensifications as a composite outcome between periods on and off OVT for the same patient.
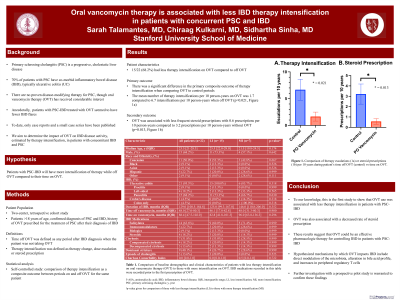
Results: 15/22 (68.2%) had less therapy intensification on OVT compared to off OVT. For our primary outcome, there was a significant difference in the number of therapy intensification events when comparing OVT to control periods. The mean number of therapy intensifications per 10 person-years on OVT was 1.7 compared to 6.7 intensifications per 10 person-years when off OVT (p=0.021, Figure 1a). For our secondary outcome, OVT was associated with less frequent steroid prescriptions with 0.6 prescriptions per 10 person-years compared to 3.2 prescriptions per 10 person-years without OVT (p=0.013, Figure 1b). See Table 1 for patient demographics.
Discussion: To our knowledge, this is the first study to show that OVT use was associated with less therapy intensification in patients with PSC-IBD. OVT was also associated with a decreased rate of steroid prescriptions. These results suggest that OVT could be an effective pharmacologic therapy for controlling IBD in patients with PSC-IBD. Hypothesized mechanisms by which OVT impacts IBD include direct modulation of the microbiota, alteration in bile acid profile, and increases in peripheral regulatory T cells. Further investigation with a prospective pilot study is warranted to confirm these findings.

Disclosures:
Sarah M. Talamantes, MD1, Chiraag Kulkarni, MD2, George Cholankeril, MD3, Touran Fardeen, BS2, Sidhartha Sinha, MD2. P3528 - Oral Vancomycin Is Associated With Less IBD Therapy Intensification in PSC-IBD, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Stanford University, Mountain View, CA; 2Stanford University, Palo Alto, CA; 3Baylor University, Houston, TX
Introduction: Primary sclerosing cholangitis (PSC) is a progressive, cholestatic liver disease. About 70% of patients with PSC have co-morbid inflammatory bowel disease (IBD), typically ulcerative colitis (UC). There is no proven disease-modifying therapy for PSC, though oral vancomycin therapy (OVT) has received considerable interest. Anecdotally, patients with PSC-IBD treated with OVT seemed to have fewer IBD flares. To date, only case reports and a small case series have been published. We aim to determine the impact of OVT on IBD disease activity, estimated by therapy intensification, in patients with concomitant IBD and PSC.
Methods: This was a two-center, retrospective, self-controlled, cohort study. The study population included patients >18 years of age, confirmed diagnosis of PSC and IBD, history of OVT prescribed for the treatment of PSC after their diagnosis of IBD. Time off OVT was defined as any period after IBD diagnosis when the patient was not taking OVT. Therapy intensification was defined as therapy change, dose escalation or steroid prescription. Patients served as their own control, comparing number of therapy intensifications as a composite outcome between periods on and off OVT for the same patient.
Results: 15/22 (68.2%) had less therapy intensification on OVT compared to off OVT. For our primary outcome, there was a significant difference in the number of therapy intensification events when comparing OVT to control periods. The mean number of therapy intensifications per 10 person-years on OVT was 1.7 compared to 6.7 intensifications per 10 person-years when off OVT (p=0.021, Figure 1a). For our secondary outcome, OVT was associated with less frequent steroid prescriptions with 0.6 prescriptions per 10 person-years compared to 3.2 prescriptions per 10 person-years without OVT (p=0.013, Figure 1b). See Table 1 for patient demographics.
Discussion: To our knowledge, this is the first study to show that OVT use was associated with less therapy intensification in patients with PSC-IBD. OVT was also associated with a decreased rate of steroid prescriptions. These results suggest that OVT could be an effective pharmacologic therapy for controlling IBD in patients with PSC-IBD. Hypothesized mechanisms by which OVT impacts IBD include direct modulation of the microbiota, alteration in bile acid profile, and increases in peripheral regulatory T cells. Further investigation with a prospective pilot study is warranted to confirm these findings.

Figure: Figure 1. Comparison of therapy escalation (a) and steroid prescriptions (b) between periods of time on and off OVT per 10 person-years of follow-up.
Disclosures:
Sarah Talamantes indicated no relevant financial relationships.
Chiraag Kulkarni indicated no relevant financial relationships.
George Cholankeril indicated no relevant financial relationships.
Touran Fardeen indicated no relevant financial relationships.
Sidhartha Sinha indicated no relevant financial relationships.
Sarah M. Talamantes, MD1, Chiraag Kulkarni, MD2, George Cholankeril, MD3, Touran Fardeen, BS2, Sidhartha Sinha, MD2. P3528 - Oral Vancomycin Is Associated With Less IBD Therapy Intensification in PSC-IBD, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
