Tuesday Poster Session
Category: IBD
P3529 - Inflammatory Bowel Disease Course May Be Less Severe in Patients After Liver Transplantation for Primary Sclerosing Cholangitis: A National Database Review
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Antoinette J. Pusateri, MD
The Ohio State University Wexner Medical Center
Columbus, OH
Presenting Author(s)
Antoinette J. Pusateri, MD, Fred Karaisz, MD, Madalina Butnariu, MD, Yevgeniya Gokun, MS, Khalid Mumtaz, MBBS
The Ohio State University Wexner Medical Center, Columbus, OH
Introduction: Data on the outcomes of inflammatory bowel disease (IBD) post liver transplant (LT) for primary sclerosing cholangitis (PSC) have been reported in small studies in the past. We explored the MarketScan database to investigate the outcomes of IBD in post-LT patients with PSC.
Methods: Adult patients older than 18 years with IBD and PSC who underwent LT between 1/1/2013 and 11/23/2020 were analyzed in the Marketscan claims database. Patients were excluded if they were in the database for less than 3 months pre-LT, had less than 6 months enrollment post-LT, or had HIV/AIDS. IBD outcomes were based on immunosuppresive medications, IBD-related surgery, and IBD-related hospitalizations. McNemar’s tests and signed rank test were used.
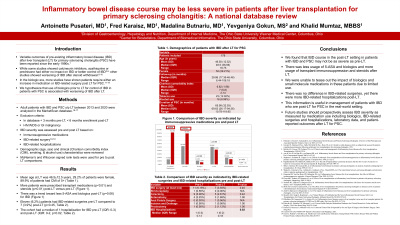
Results: A total of 178 patients with IBD and PSC with mean age at LT of 46.5±12.5 years, 29.2% female were studied. Median follow up was 29.86 months. Pre-LT 94 (52.8%) patients were on steroids, 90 (50.5%) were on 5-ASA, 35 (19.6%) were on antimetabolites, 20 (11.2%) were on biologics, 1 (0.5%) was on small molecules for IBD and 26 (14.61%) were on transplant medications. Post-LT 159 (89.3%) patients were on steroids, 76 (42.7%) on 5-ASA, 27 (15.1%) on antimetabolites, 11 (6.2%) on biologics, none on small molecules for IBD and 164 (92.13%) were on transplant medications. As expected, more patients were prescribed transplant medications (p< 0.0001) and steroids (p < 0.001) post-LT as compared to pre-LT. There was a trend toward less 5-ASA and biologics used post-LT (p=0.06) for IBD. Eleven (6.2%) patients had IBD-related surgeries pre-LT compared to 7 (3.9%) post-LT (p=0.45). The cohort had a median of 1 hospitalization (IQR: 0-3) for IBD pre-LT and a median of 1 hospitalization (IQR: 0-2) post-LT (p=0.02, Table 1).
Discussion: We found that IBD course in the post-LT setting in patients with IBD and PSC may not be as severe as pre-LT, as reflected by a trend in less use of 5-ASA and biologics and less IBD-related hospitalizations. We were unable to tease out the impact of biologics and small molecule medications in these patients due to their limited use in this cohort. This information is useful in management of patients with IBD who are post-LT for PSC in the real-world setting.
Disclosures:
Antoinette J. Pusateri, MD, Fred Karaisz, MD, Madalina Butnariu, MD, Yevgeniya Gokun, MS, Khalid Mumtaz, MBBS. P3529 - Inflammatory Bowel Disease Course May Be Less Severe in Patients After Liver Transplantation for Primary Sclerosing Cholangitis: A National Database Review, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
The Ohio State University Wexner Medical Center, Columbus, OH
Introduction: Data on the outcomes of inflammatory bowel disease (IBD) post liver transplant (LT) for primary sclerosing cholangitis (PSC) have been reported in small studies in the past. We explored the MarketScan database to investigate the outcomes of IBD in post-LT patients with PSC.
Methods: Adult patients older than 18 years with IBD and PSC who underwent LT between 1/1/2013 and 11/23/2020 were analyzed in the Marketscan claims database. Patients were excluded if they were in the database for less than 3 months pre-LT, had less than 6 months enrollment post-LT, or had HIV/AIDS. IBD outcomes were based on immunosuppresive medications, IBD-related surgery, and IBD-related hospitalizations. McNemar’s tests and signed rank test were used.
Results: A total of 178 patients with IBD and PSC with mean age at LT of 46.5±12.5 years, 29.2% female were studied. Median follow up was 29.86 months. Pre-LT 94 (52.8%) patients were on steroids, 90 (50.5%) were on 5-ASA, 35 (19.6%) were on antimetabolites, 20 (11.2%) were on biologics, 1 (0.5%) was on small molecules for IBD and 26 (14.61%) were on transplant medications. Post-LT 159 (89.3%) patients were on steroids, 76 (42.7%) on 5-ASA, 27 (15.1%) on antimetabolites, 11 (6.2%) on biologics, none on small molecules for IBD and 164 (92.13%) were on transplant medications. As expected, more patients were prescribed transplant medications (p< 0.0001) and steroids (p < 0.001) post-LT as compared to pre-LT. There was a trend toward less 5-ASA and biologics used post-LT (p=0.06) for IBD. Eleven (6.2%) patients had IBD-related surgeries pre-LT compared to 7 (3.9%) post-LT (p=0.45). The cohort had a median of 1 hospitalization (IQR: 0-3) for IBD pre-LT and a median of 1 hospitalization (IQR: 0-2) post-LT (p=0.02, Table 1).
Discussion: We found that IBD course in the post-LT setting in patients with IBD and PSC may not be as severe as pre-LT, as reflected by a trend in less use of 5-ASA and biologics and less IBD-related hospitalizations. We were unable to tease out the impact of biologics and small molecule medications in these patients due to their limited use in this cohort. This information is useful in management of patients with IBD who are post-LT for PSC in the real-world setting.
Disclosures:
Antoinette Pusateri indicated no relevant financial relationships.
Fred Karaisz indicated no relevant financial relationships.
Madalina Butnariu indicated no relevant financial relationships.
Yevgeniya Gokun indicated no relevant financial relationships.
Khalid Mumtaz indicated no relevant financial relationships.
Antoinette J. Pusateri, MD, Fred Karaisz, MD, Madalina Butnariu, MD, Yevgeniya Gokun, MS, Khalid Mumtaz, MBBS. P3529 - Inflammatory Bowel Disease Course May Be Less Severe in Patients After Liver Transplantation for Primary Sclerosing Cholangitis: A National Database Review, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
