Tuesday Poster Session
Category: IBD
P3540 - Colonoscopy Prep Is Associated With Increased Risk of Flare Among Patients With Previously Inactive Inflammatory Bowel Disease
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- CK
Chiraag Kulkarni, MD
Stanford University
Palo Alto, California
Presenting Author(s)
Chiraag Kulkarni, MD1, Sarah M. Talamantes, MD2, Sidhartha Sinha, MD1
1Stanford University, Palo Alto, CA; 2Stanford University, Mountain View, CA
Introduction: Patients with inflammatory bowel disease (IBD) have an approximately 3-fold increased risk of colorectal cancer (CRC) death and undergo frequent surveillance via colonoscopy. Anecdotal evidence and small studies suggest an increased risk of flare after colonoscopy. However, we lack data from large studies, and it is unknown whether IBD patients without active disease who undergo colonoscopy for CRC surveillance are truly at increased risk of IBD flare.
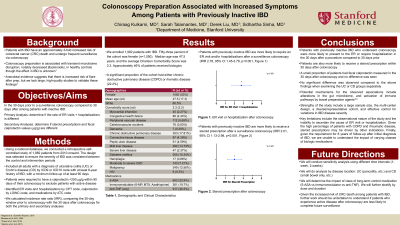
Methods: We conducted a retrospective, self-controlled study of 1,982 patients using a national database. Our study population included a cohort of men and women greater than 18 years of age who had a diagnosis of either ulcerative colitis or Crohn’s disease. In order to exclude patients undergoing colonoscopy for suspicion of active disease, patients were required to have a calprotectin less than 250 ug/g within 90 days of their colonoscopy. Furthermore, only patients who underwent colonoscopy for purposes of colorectal cancer screening or surveillance were included. Our primary outcome was a composite of emergency room (ER) visit or hospitalization for IBD. As a secondary outcome, we measured rates of steroid prescription. We evaluated both outcomes comparing the 30-day period prior to colonoscopy with the 30-day period after colonoscopy.
Results: Fifty three percent of the cohort was female (n=1,050) with a median age of 42.6 years. Forty one percent of patients in the cohort were receiving biologic therapy for their IBD. Patients with IBD who underwent colonoscopy were more likely to present to the ER or require hospitalization for IBD after the procedure, with an incident rate ratio (IRR) of 2.76 (1.45-3.78, p< 0.001, e-value 2.4). Patients were also more likely to receive a steroid prescription within 30-days after colonoscopy, with an IRR of 2.01 (1.13-2.98, p< 0.001).
Discussion: We show that patients with quiescent IBD who undergo colonoscopy for colorectal cancer surveillance are more likely have an ER visit or hospitalization for IBD following the procedure. Potential mechanism for this association includes alterations in the gut microbiome, and activation of immune pathways by bowel preparation agents. Given the increased risk of CRC death among patients with IBD, further work should be undertaken to understand if patients who experience active disease after colonoscopy are less likely to complete to future CRC surveillance colonoscopy.
Disclosures:
Chiraag Kulkarni, MD1, Sarah M. Talamantes, MD2, Sidhartha Sinha, MD1. P3540 - Colonoscopy Prep Is Associated With Increased Risk of Flare Among Patients With Previously Inactive Inflammatory Bowel Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Stanford University, Palo Alto, CA; 2Stanford University, Mountain View, CA
Introduction: Patients with inflammatory bowel disease (IBD) have an approximately 3-fold increased risk of colorectal cancer (CRC) death and undergo frequent surveillance via colonoscopy. Anecdotal evidence and small studies suggest an increased risk of flare after colonoscopy. However, we lack data from large studies, and it is unknown whether IBD patients without active disease who undergo colonoscopy for CRC surveillance are truly at increased risk of IBD flare.
Methods: We conducted a retrospective, self-controlled study of 1,982 patients using a national database. Our study population included a cohort of men and women greater than 18 years of age who had a diagnosis of either ulcerative colitis or Crohn’s disease. In order to exclude patients undergoing colonoscopy for suspicion of active disease, patients were required to have a calprotectin less than 250 ug/g within 90 days of their colonoscopy. Furthermore, only patients who underwent colonoscopy for purposes of colorectal cancer screening or surveillance were included. Our primary outcome was a composite of emergency room (ER) visit or hospitalization for IBD. As a secondary outcome, we measured rates of steroid prescription. We evaluated both outcomes comparing the 30-day period prior to colonoscopy with the 30-day period after colonoscopy.
Results: Fifty three percent of the cohort was female (n=1,050) with a median age of 42.6 years. Forty one percent of patients in the cohort were receiving biologic therapy for their IBD. Patients with IBD who underwent colonoscopy were more likely to present to the ER or require hospitalization for IBD after the procedure, with an incident rate ratio (IRR) of 2.76 (1.45-3.78, p< 0.001, e-value 2.4). Patients were also more likely to receive a steroid prescription within 30-days after colonoscopy, with an IRR of 2.01 (1.13-2.98, p< 0.001).
Discussion: We show that patients with quiescent IBD who undergo colonoscopy for colorectal cancer surveillance are more likely have an ER visit or hospitalization for IBD following the procedure. Potential mechanism for this association includes alterations in the gut microbiome, and activation of immune pathways by bowel preparation agents. Given the increased risk of CRC death among patients with IBD, further work should be undertaken to understand if patients who experience active disease after colonoscopy are less likely to complete to future CRC surveillance colonoscopy.
Disclosures:
Chiraag Kulkarni indicated no relevant financial relationships.
Sarah Talamantes indicated no relevant financial relationships.
Sidhartha Sinha indicated no relevant financial relationships.
Chiraag Kulkarni, MD1, Sarah M. Talamantes, MD2, Sidhartha Sinha, MD1. P3540 - Colonoscopy Prep Is Associated With Increased Risk of Flare Among Patients With Previously Inactive Inflammatory Bowel Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
