Tuesday Poster Session
Category: IBD
P3557 - Older Adult-Onset of Inflammatory Bowel Diseases Is Associated With Higher Utilization of Analgesic Medications Within 1 Year After Diagnosis: A Danish Nationwide Cohort Study Between 1996-2021
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- RD
Rahul Dalal, MD, MPH
Brigham and Women's Hospital, Harvard Medical School
Boston, MA
Presenting Author(s)
Rahul Dalal, MD, MPH1, Bente Mertz Nørgård, MD, DMSc, PhD2, Floor Zegers, MSc2, Jens Kjedlsen, MD, PhD3, Sonia Friedman, MD4, Jessica R.. Allegretti, MD, MPH1, Ken Lund, MSc, PhD2
1Brigham and Women's Hospital, Harvard Medical School, Boston, MA; 2Center for Clinical Epidemiology, Odense University Hospital, and Research Unit of Clinical Epidemiology, University of Southern Denmark, Odense, Syddanmark, Denmark; 3University of Southern Denmark, Odense, Syddanmark, Denmark; 4Tufts University School of Medicine, Boston, MA
Introduction: Recent nationwide data suggests that adults diagnosed with inflammatory bowel disease (IBD) at an older age are less likely to utilize disease modifying therapies. Utilization of analgesics, many of which are associated with harmful complications in older adults, is poorly understood with regards to age of IBD onset.
Methods: This nationwide, registry-based cohort study included adults diagnosed with IBD between 1996-2021 in Denmark. To define a cohort where analgesics prescribed within 1 yr after IBD diagnosis may be more likely for IBD-related pain, the following patients were excluded: those who died within 1 yr after IBD diagnosis, those with musculoskeletal diseases or cancer diagnoses within 1 yr before IBD diagnosis, and those prescribed analgesics within 1 yr before IBD diagnosis (except 3 months before IBD diagnosis). The cohort was stratified by age of IBD onset: 18-39 yrs (young adult), 40-59 yrs (adult), and 60+ yrs (older adult). We examined the proportion of patients who received analgesic prescriptions within 1 yr after IBD diagnosis: strong opioids (SOs), tramadol, codeine, NSAIDs, and paracetamol. Multivariable logistic regression was performed to determine associations between age of IBD onset with SO prescriptions and the composite of SO/tramadol/codeine prescriptions.
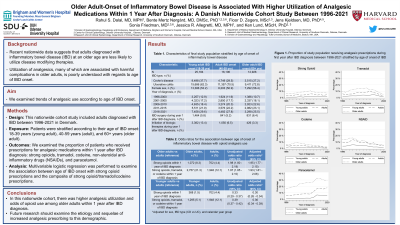
Results: The study included 25,184 (46.5%) young adults, 16,106 (29.7%) adults, and 12,926 (23.8%) older adults at IBD onset. Cohort characteristics are presented in Table 1. Older adults most commonly utilized analgesics of each class: 8.3% SOs, 11.7% tramadol, 5.7% codeine, 10.6% NSAIDs, 25.7% paracetamol (Table 1, Fig 1). Results were similar after excluding those who underwent IBD surgery within 1 yr after diagnosis (Table 1). Between 1996-2021, prescriptions of SOs, tramadol, and codeine were stable, paracetamol increased, and NSAIDs decreased in all age groups (Fig 1). Older adults had higher adjusted odds of receiving SO prescriptions (aOR 1.95, 95% CI 1.77-2.15) and the composite of SO/tramadol/codeine prescriptions (aOR 1.93, 95% CI 1.81-2.06) within 1 yr after IBD diagnosis vs adults. Younger adults had lower adjusted odds of these outcomes, respectively, vs adults (aOR 0.30, 95% CI 0.26-0.34; aOR 0.36, 95% CI 0.34-0.39).
Discussion: In this nationwide cohort, there was higher analgesic utilization and odds of opioid use among older adults within 1 yr after IBD diagnosis. Additional research is needed to examine the etiology and sequelae of increased analgesic prescribing to this demographic.

Disclosures:
Rahul Dalal, MD, MPH1, Bente Mertz Nørgård, MD, DMSc, PhD2, Floor Zegers, MSc2, Jens Kjedlsen, MD, PhD3, Sonia Friedman, MD4, Jessica R.. Allegretti, MD, MPH1, Ken Lund, MSc, PhD2. P3557 - Older Adult-Onset of Inflammatory Bowel Diseases Is Associated With Higher Utilization of Analgesic Medications Within 1 Year After Diagnosis: A Danish Nationwide Cohort Study Between 1996-2021, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Brigham and Women's Hospital, Harvard Medical School, Boston, MA; 2Center for Clinical Epidemiology, Odense University Hospital, and Research Unit of Clinical Epidemiology, University of Southern Denmark, Odense, Syddanmark, Denmark; 3University of Southern Denmark, Odense, Syddanmark, Denmark; 4Tufts University School of Medicine, Boston, MA
Introduction: Recent nationwide data suggests that adults diagnosed with inflammatory bowel disease (IBD) at an older age are less likely to utilize disease modifying therapies. Utilization of analgesics, many of which are associated with harmful complications in older adults, is poorly understood with regards to age of IBD onset.
Methods: This nationwide, registry-based cohort study included adults diagnosed with IBD between 1996-2021 in Denmark. To define a cohort where analgesics prescribed within 1 yr after IBD diagnosis may be more likely for IBD-related pain, the following patients were excluded: those who died within 1 yr after IBD diagnosis, those with musculoskeletal diseases or cancer diagnoses within 1 yr before IBD diagnosis, and those prescribed analgesics within 1 yr before IBD diagnosis (except 3 months before IBD diagnosis). The cohort was stratified by age of IBD onset: 18-39 yrs (young adult), 40-59 yrs (adult), and 60+ yrs (older adult). We examined the proportion of patients who received analgesic prescriptions within 1 yr after IBD diagnosis: strong opioids (SOs), tramadol, codeine, NSAIDs, and paracetamol. Multivariable logistic regression was performed to determine associations between age of IBD onset with SO prescriptions and the composite of SO/tramadol/codeine prescriptions.
Results: The study included 25,184 (46.5%) young adults, 16,106 (29.7%) adults, and 12,926 (23.8%) older adults at IBD onset. Cohort characteristics are presented in Table 1. Older adults most commonly utilized analgesics of each class: 8.3% SOs, 11.7% tramadol, 5.7% codeine, 10.6% NSAIDs, 25.7% paracetamol (Table 1, Fig 1). Results were similar after excluding those who underwent IBD surgery within 1 yr after diagnosis (Table 1). Between 1996-2021, prescriptions of SOs, tramadol, and codeine were stable, paracetamol increased, and NSAIDs decreased in all age groups (Fig 1). Older adults had higher adjusted odds of receiving SO prescriptions (aOR 1.95, 95% CI 1.77-2.15) and the composite of SO/tramadol/codeine prescriptions (aOR 1.93, 95% CI 1.81-2.06) within 1 yr after IBD diagnosis vs adults. Younger adults had lower adjusted odds of these outcomes, respectively, vs adults (aOR 0.30, 95% CI 0.26-0.34; aOR 0.36, 95% CI 0.34-0.39).
Discussion: In this nationwide cohort, there was higher analgesic utilization and odds of opioid use among older adults within 1 yr after IBD diagnosis. Additional research is needed to examine the etiology and sequelae of increased analgesic prescribing to this demographic.

Figure: Figure 1. Proportion of study population receiving analgesic prescriptions during first year after IBD diagnosis between 1996-2021
Disclosures:
Rahul Dalal: Centaur Labs – Consultant. Janssen – Consultant, Grant/Research Support. Pfizer – Grant/Research Support.
Bente Mertz Nørgård indicated no relevant financial relationships.
Floor Zegers indicated no relevant financial relationships.
Jens Kjedlsen indicated no relevant financial relationships.
Sonia Friedman indicated no relevant financial relationships.
Jessica Allegretti: Abbvie – Consultant, Speakers Bureau. Adiso Therapeutics – Consultant. Artizan – Consultant. Artugen Therapeutics – Consultant. Baccain – Consultant. Bristol-Myers Squibb/Celgene – Consultant, Speakers Bureau. Ferring Pharmaceuticals – Consultant. Finch Therapeutics – Consultant. Iterative Scopes – Consultant. Janssen – Consultant, Grant/Research Support, Speakers Bureau. Merck – Consultant, Grant/Research Support. Morphic – Consultant. Pandion Therapeutics – Consultant. Pfizer – Consultant, Grant/Research Support. Roivant Sciences – Consultant. Seres Therapeutics – Consultant. Servatus – Consultant. Summit – Consultant.
Ken Lund indicated no relevant financial relationships.
Rahul Dalal, MD, MPH1, Bente Mertz Nørgård, MD, DMSc, PhD2, Floor Zegers, MSc2, Jens Kjedlsen, MD, PhD3, Sonia Friedman, MD4, Jessica R.. Allegretti, MD, MPH1, Ken Lund, MSc, PhD2. P3557 - Older Adult-Onset of Inflammatory Bowel Diseases Is Associated With Higher Utilization of Analgesic Medications Within 1 Year After Diagnosis: A Danish Nationwide Cohort Study Between 1996-2021, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
