Tuesday Poster Session
Category: IBD
P3564 - Racial and Socioeconomic Diversity and Impediments to Care of Crohn’s Disease Patients at an Urban Medical Center
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- PK
Paul Kim, BA
Wayne State University School of Medicine
Detroit, MI
Presenting Author(s)
Paul Kim, BA1, Angy Hanna, MD2, Jing Wang, MD3, Bashar Mohamad, MD4, Paul H. Naylor, PhD5, Milton G. Mutchnick, MD1
1Wayne State University School of Medicine, Detroit, MI; 2Detroit Medical Center, Detroit, MI; 3Detroit Medical Center/Wayne State University, Detroit, MI; 4Wayne State University, Detroit, MI; 5Wayne State University School of Medicine, Hazel Park, MI
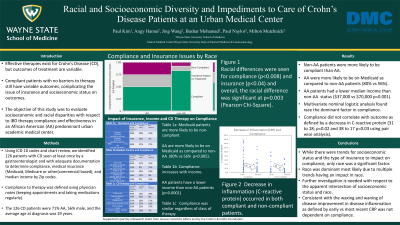
Introduction: Effective therapies exist for Crohn’s Disease (CD) but outcomes of treatment are variable. Compliant patients with no barriers to therapy still have variable outcomes, complicating the issue of insurance and socioeconomic status on outcomes. The objective of this study was to evaluate socioeconomic and racial disparity with respect to IBD therapy compliance and effectiveness in an African American (AA) predominant urban medical center.
Methods: We identified 126 patients with CD seen at least once by a gastroenterologist and with adequate documentation to determine compliance, medical insurance (Medicaid, Medicare or other), and median income by Zip codes. Compliance to therapy was defined using physician notes (keeping appointments and taking medications regularly).
Results: The 126 CD patients were 71% AA, 56% male, and the average age at diagnosis was 29 years. As shown in figure 1anad table 1, the most significant observation was that AA patients with CD were less likely to be compliant as compared to non-AA (50% vs 84%). They were also more likely to have an insurance impact on treatment (24% vs 8%). When the % of patients with Medicaid were evaluated by race, AA were more likely to be on Medicaid as compared to non-AA patients (80% vs 56%). When socioeconomic status by Zip code defined median income was evaluated by race, AA patients had a lower status ($37,000 vs $70,000 p=0.001). When income and compliance regardless of race was evaluated, it was not different ($50,000 vs $44,000 p=0.32) (Table 1). This was also true for insurance effect on compliance and the class of CD therapy (Table 1). When subjected to multivariate nominal logistic analysis, race remained the dominant significant factor in compliance (last column in Table 1). With respect to compliance and outcomes (inflammation as defined by C-reactive protein (mg/L) at earliest and most recent time points), the average decrease was similar between compliant and non-compliant patients (31 to 18; p=0.02 and 38 to 17 p=0.03 using pair wise analysis).
Discussion: While there were trends for socioeconomic status and the type of insurance to impact on compliance, only race was a significant factor. Further investigation is needed with respect to the apparent intersection of socioeconomic status and race. Consistent with the waxing and waning of CD in even therapy compliant patients, improvement in disease inflammation as defined by early vs most recent CRP was not dependent on compliance.

Disclosures:
Paul Kim, BA1, Angy Hanna, MD2, Jing Wang, MD3, Bashar Mohamad, MD4, Paul H. Naylor, PhD5, Milton G. Mutchnick, MD1. P3564 - Racial and Socioeconomic Diversity and Impediments to Care of Crohn’s Disease Patients at an Urban Medical Center, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Wayne State University School of Medicine, Detroit, MI; 2Detroit Medical Center, Detroit, MI; 3Detroit Medical Center/Wayne State University, Detroit, MI; 4Wayne State University, Detroit, MI; 5Wayne State University School of Medicine, Hazel Park, MI
Introduction: Effective therapies exist for Crohn’s Disease (CD) but outcomes of treatment are variable. Compliant patients with no barriers to therapy still have variable outcomes, complicating the issue of insurance and socioeconomic status on outcomes. The objective of this study was to evaluate socioeconomic and racial disparity with respect to IBD therapy compliance and effectiveness in an African American (AA) predominant urban medical center.
Methods: We identified 126 patients with CD seen at least once by a gastroenterologist and with adequate documentation to determine compliance, medical insurance (Medicaid, Medicare or other), and median income by Zip codes. Compliance to therapy was defined using physician notes (keeping appointments and taking medications regularly).
Results: The 126 CD patients were 71% AA, 56% male, and the average age at diagnosis was 29 years. As shown in figure 1anad table 1, the most significant observation was that AA patients with CD were less likely to be compliant as compared to non-AA (50% vs 84%). They were also more likely to have an insurance impact on treatment (24% vs 8%). When the % of patients with Medicaid were evaluated by race, AA were more likely to be on Medicaid as compared to non-AA patients (80% vs 56%). When socioeconomic status by Zip code defined median income was evaluated by race, AA patients had a lower status ($37,000 vs $70,000 p=0.001). When income and compliance regardless of race was evaluated, it was not different ($50,000 vs $44,000 p=0.32) (Table 1). This was also true for insurance effect on compliance and the class of CD therapy (Table 1). When subjected to multivariate nominal logistic analysis, race remained the dominant significant factor in compliance (last column in Table 1). With respect to compliance and outcomes (inflammation as defined by C-reactive protein (mg/L) at earliest and most recent time points), the average decrease was similar between compliant and non-compliant patients (31 to 18; p=0.02 and 38 to 17 p=0.03 using pair wise analysis).
Discussion: While there were trends for socioeconomic status and the type of insurance to impact on compliance, only race was a significant factor. Further investigation is needed with respect to the apparent intersection of socioeconomic status and race. Consistent with the waxing and waning of CD in even therapy compliant patients, improvement in disease inflammation as defined by early vs most recent CRP was not dependent on compliance.

Figure: Figure 1 Impact of race on compliance. The effect of the race of the CD patients on therapy was evaluated with respect to Compliance (regular visits and drug compliance) vs Non-compliance. Also plotted are patients where insurance had an impact on treatment. Racial differences were seen for compliance (p<0.008) and insurance (p<0.04) and overall, the racial difference was significant at p=0.003 (Pearson Chi-Square).
Disclosures:
Paul Kim indicated no relevant financial relationships.
Angy Hanna indicated no relevant financial relationships.
Jing Wang indicated no relevant financial relationships.
Bashar Mohamad indicated no relevant financial relationships.
Paul Naylor: Janssen Biotech Inc – Grant/Research Support.
Milton Mutchnick: Chronic Liver Disease Foundation – Speakers Bureau. Janssen Biotech Inc – Grant/Research Support.
Paul Kim, BA1, Angy Hanna, MD2, Jing Wang, MD3, Bashar Mohamad, MD4, Paul H. Naylor, PhD5, Milton G. Mutchnick, MD1. P3564 - Racial and Socioeconomic Diversity and Impediments to Care of Crohn’s Disease Patients at an Urban Medical Center, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
