Tuesday Poster Session
Category: IBD
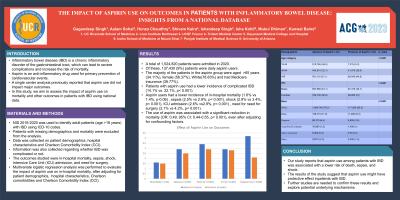
P3566 - The Impact of Aspirin Use on Outcomes in Patients with Inflammatory Bowel Disease: Insights from a National Database
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
Gagandeep Singh Arora, MD
UC Riverside School of Medicine
San Bernardino, CA
Presenting Author(s)
Gagandeep Singh Arora, MD1, Aalam Sohal, MD2, Hunza Chaudhry, MD3, Shivam Kalra, MBBS4, Ishandeep Singh, MBBS5, Isha Kohli, MBBS, CPH, MPH6, Mukul Dhiman, MBBS7, Kanwal Bains, MBBS, CNSC8
1UC Riverside School of Medicine, San Bernardino, CA; 2Liver Institute Northwest, Seattle, WA; 3University of California San Francisco, Fresno, CA; 4Trident Medical Center, Charleston, SC; 5Dayanand Medical College and Hospital, Ludhiana, Punjab, India; 6Icahn School of Medicine at Mount Sinai, New York, NY; 7Punjab Institute of Medical Sciences, Jalandhar, Kharar, Punjab, India; 8University of Arizona, Tucson, AZ
Introduction: Inflammatory bowel disease (IBD) is a chronic inflammatory disorder of the gastrointestinal tract, which can lead to severe complications and increase the risk of mortality. Aspirin is an anti-inflammatory drug used for primary prevention of cardiovascular events. A single center analysis previously reported that aspirin use did not impact major outcomes. In this study, we aim to assess the impact of aspirin use on mortality and other outcomes in patients with IBD using national data.
Methods: NIS 2016-2020 was used to identify adult patients(age >18 years) with IBD using ICD-10 codes. Patients with missing demographics and mortality were excluded from the analysis. Data was collected on patient demographics, hospital characteristics, Charlson Comorbidity Index (CCI), and Charlson comorbidities. Information was also collected regarding whether IBD was complicated or not. The outcomes studied were in-hospital mortality, sepsis, shock, Intensive Care Unit (ICU) admission, and need for surgery. Multivariate logistic regression analysis was performed to evaluate the impact of aspirin use on in-hospital mortality, after adjusting for patient demographics, hospital characteristics, Charlson comorbidities and Charlson Comorbidity Index (CCI).
Results: A total of 1,524,820 patients were admitted in 2020. Of these, 137,430 (9%) patients were daily aspirin users. The majority of the patients in the aspirin group were aged >65 years (34.11%), female (56.37%), White (78.83%) and had Medicare insurance (36.77%). Patients with aspirin use had a lower incidence of complicated IBD (14.1% vs. 22.1%, p< 0.001). Aspirin users had a lower incidence of in-hospital mortality (1.6% vs 1.4%, p-0.06) , sepsis (2.5% vs 2.9%, p< 0.001), shock (2.9% vs 3.4%, p< 0.001), ICU admission (2.6% vs 2.9%, p< 0.001) , need for need for surgery (2.1% vs 4.2%, p< 0.001). The use of aspirin was associated with a significant reduction in mortality (OR: 0.49, 95% CI: 0.44-0.55, p< 0.001), even after adjusting for confounding factors.
Discussion: Our study reports that aspirin use among patients with IBD was associated with a lower risk of death, sepsis, and shock. The results of the study suggest that aspirin use might have protective effect in patients with IBD.Further studies are needed to confirm these results and explore potential underlying mechanisms.

Disclosures:
Gagandeep Singh Arora, MD1, Aalam Sohal, MD2, Hunza Chaudhry, MD3, Shivam Kalra, MBBS4, Ishandeep Singh, MBBS5, Isha Kohli, MBBS, CPH, MPH6, Mukul Dhiman, MBBS7, Kanwal Bains, MBBS, CNSC8. P3566 - The Impact of Aspirin Use on Outcomes in Patients with Inflammatory Bowel Disease: Insights from a National Database, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1UC Riverside School of Medicine, San Bernardino, CA; 2Liver Institute Northwest, Seattle, WA; 3University of California San Francisco, Fresno, CA; 4Trident Medical Center, Charleston, SC; 5Dayanand Medical College and Hospital, Ludhiana, Punjab, India; 6Icahn School of Medicine at Mount Sinai, New York, NY; 7Punjab Institute of Medical Sciences, Jalandhar, Kharar, Punjab, India; 8University of Arizona, Tucson, AZ
Introduction: Inflammatory bowel disease (IBD) is a chronic inflammatory disorder of the gastrointestinal tract, which can lead to severe complications and increase the risk of mortality. Aspirin is an anti-inflammatory drug used for primary prevention of cardiovascular events. A single center analysis previously reported that aspirin use did not impact major outcomes. In this study, we aim to assess the impact of aspirin use on mortality and other outcomes in patients with IBD using national data.
Methods: NIS 2016-2020 was used to identify adult patients(age >18 years) with IBD using ICD-10 codes. Patients with missing demographics and mortality were excluded from the analysis. Data was collected on patient demographics, hospital characteristics, Charlson Comorbidity Index (CCI), and Charlson comorbidities. Information was also collected regarding whether IBD was complicated or not. The outcomes studied were in-hospital mortality, sepsis, shock, Intensive Care Unit (ICU) admission, and need for surgery. Multivariate logistic regression analysis was performed to evaluate the impact of aspirin use on in-hospital mortality, after adjusting for patient demographics, hospital characteristics, Charlson comorbidities and Charlson Comorbidity Index (CCI).
Results: A total of 1,524,820 patients were admitted in 2020. Of these, 137,430 (9%) patients were daily aspirin users. The majority of the patients in the aspirin group were aged >65 years (34.11%), female (56.37%), White (78.83%) and had Medicare insurance (36.77%). Patients with aspirin use had a lower incidence of complicated IBD (14.1% vs. 22.1%, p< 0.001). Aspirin users had a lower incidence of in-hospital mortality (1.6% vs 1.4%, p-0.06) , sepsis (2.5% vs 2.9%, p< 0.001), shock (2.9% vs 3.4%, p< 0.001), ICU admission (2.6% vs 2.9%, p< 0.001) , need for need for surgery (2.1% vs 4.2%, p< 0.001). The use of aspirin was associated with a significant reduction in mortality (OR: 0.49, 95% CI: 0.44-0.55, p< 0.001), even after adjusting for confounding factors.
Discussion: Our study reports that aspirin use among patients with IBD was associated with a lower risk of death, sepsis, and shock. The results of the study suggest that aspirin use might have protective effect in patients with IBD.Further studies are needed to confirm these results and explore potential underlying mechanisms.

Figure: Effect of Aspirin Use on Outcomes
Disclosures:
Gagandeep Singh Arora indicated no relevant financial relationships.
Aalam Sohal indicated no relevant financial relationships.
Hunza Chaudhry indicated no relevant financial relationships.
Shivam Kalra indicated no relevant financial relationships.
Ishandeep Singh indicated no relevant financial relationships.
Isha Kohli indicated no relevant financial relationships.
Mukul Dhiman indicated no relevant financial relationships.
Kanwal Bains indicated no relevant financial relationships.
Gagandeep Singh Arora, MD1, Aalam Sohal, MD2, Hunza Chaudhry, MD3, Shivam Kalra, MBBS4, Ishandeep Singh, MBBS5, Isha Kohli, MBBS, CPH, MPH6, Mukul Dhiman, MBBS7, Kanwal Bains, MBBS, CNSC8. P3566 - The Impact of Aspirin Use on Outcomes in Patients with Inflammatory Bowel Disease: Insights from a National Database, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
