Tuesday Poster Session
Category: IBD
P3567 - Impact of Gastrointestinal PCR in Patients With Ileal Pouch-Anal Anastomosis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Kate E. Lee, MD, MS
Duke University Medical Center
Durham, NC
Presenting Author(s)
Kate E. Lee, MD, MS1, Zainab Aziz, BA, BS2, Charu Vyas, BA2, Connor Barrett, BA2, Amy Hembree, MD2, Joshua Gray, MD1, Nathan Suek, MD2, Hueyjong Shih, MD2, Michael Artin, MD2, Priya Sehgal, MD, MPH, MS2, Adam S. Faye, MD, MS3, Bo Shen, MD, FACG2
1Duke University Medical Center, Durham, NC; 2Columbia University Medical Center, New York, NY; 3New York University Langone Health, New York, NY
Introduction: An estimated 20-50% of patients with ileal pouch-anal anastomosis (IPAA) develop pouchitis. Pouchitis may result from dysbiosis or infection, typically presents with increased stool frequency and urgency, and is often treated with antibiotics. Specific pathogens detected on multiplex gastrointestinal (GI) PCR can contribute to the development of pouchitis. However, the prevalence and impact of a positive GI pathogen contributing to pouchitis is unknown.
Methods: Retrospective cohort study of 60 patients with IPAA at Columbia University Medical Center between April 1, 2015 and May 23, 2022. The electronic medical record was searched for patients with IPAA who had positive GI PCR; 20 cases were identified, and compared with 40 controls who were randomly selected from the cohort of IPAA patients with negative GI PCR. Three cases and 3 controls with familial adenomatous polyposis were included. Chart review confirmed inclusion criteria and collection of risk factors, and outcomes included symptom recurrence and hospitalization. Descriptive statistics and univariate analyses using chi-square, Fisher’s exact, and Wilcoxon rank-sum tests were performed.
Results: Of 1133 pouch patients who underwent GI PCR, 20 (1.8%) tested positive. The most frequent pathogens included Norovirus (30%), Clostridioides difficile (25%), Yersinia enterocolitica (10%), and Enteropathogenic E. coli (10%) (Figure 1). No patients had more than one pathogen detected. Of patients with positive GI PCR, 8 (40%) presented with increased stool frequency, 4 (20%) with rectal bleeding, and 7 (35%) with increased fecal urgency. Of those with negative GI PCR, 15 (37.5%) presented with increased stool frequency, 3 (7.5%) with rectal bleeding, and 18 (45%) with increased fecal urgency. Overall, 13 (65%) patients with positive GI PCR were treated with antibiotics, compared to 12 (30%) with negative GI PCR, OR 4.3, p=0.01 (Table 1). Positive GI PCR was not associated with symptom recurrence, hospitalization or sepsis or intensive care unit admission within 3 months, or repeat surgery due to pouchitis.
Discussion: The yield of GI PCR for bacterial pathogens in patients with IPAA was low at 1.8%, similar to a previously reported 1.7% for stool culture in IPAA patients. Although patients with positive GI PCR were significantly more likely to be treated with antibiotics, they did not have differences in positive or negative clinical outcomes studied. Further studies should investigate the utility of GI PCR in pouchitis management.

Disclosures:
Kate E. Lee, MD, MS1, Zainab Aziz, BA, BS2, Charu Vyas, BA2, Connor Barrett, BA2, Amy Hembree, MD2, Joshua Gray, MD1, Nathan Suek, MD2, Hueyjong Shih, MD2, Michael Artin, MD2, Priya Sehgal, MD, MPH, MS2, Adam S. Faye, MD, MS3, Bo Shen, MD, FACG2. P3567 - Impact of Gastrointestinal PCR in Patients With Ileal Pouch-Anal Anastomosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Duke University Medical Center, Durham, NC; 2Columbia University Medical Center, New York, NY; 3New York University Langone Health, New York, NY
Introduction: An estimated 20-50% of patients with ileal pouch-anal anastomosis (IPAA) develop pouchitis. Pouchitis may result from dysbiosis or infection, typically presents with increased stool frequency and urgency, and is often treated with antibiotics. Specific pathogens detected on multiplex gastrointestinal (GI) PCR can contribute to the development of pouchitis. However, the prevalence and impact of a positive GI pathogen contributing to pouchitis is unknown.
Methods: Retrospective cohort study of 60 patients with IPAA at Columbia University Medical Center between April 1, 2015 and May 23, 2022. The electronic medical record was searched for patients with IPAA who had positive GI PCR; 20 cases were identified, and compared with 40 controls who were randomly selected from the cohort of IPAA patients with negative GI PCR. Three cases and 3 controls with familial adenomatous polyposis were included. Chart review confirmed inclusion criteria and collection of risk factors, and outcomes included symptom recurrence and hospitalization. Descriptive statistics and univariate analyses using chi-square, Fisher’s exact, and Wilcoxon rank-sum tests were performed.
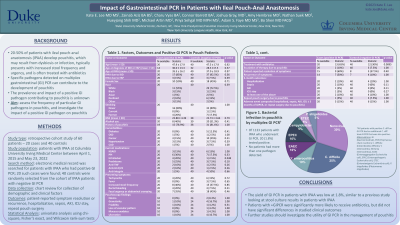
Results: Of 1133 pouch patients who underwent GI PCR, 20 (1.8%) tested positive. The most frequent pathogens included Norovirus (30%), Clostridioides difficile (25%), Yersinia enterocolitica (10%), and Enteropathogenic E. coli (10%) (Figure 1). No patients had more than one pathogen detected. Of patients with positive GI PCR, 8 (40%) presented with increased stool frequency, 4 (20%) with rectal bleeding, and 7 (35%) with increased fecal urgency. Of those with negative GI PCR, 15 (37.5%) presented with increased stool frequency, 3 (7.5%) with rectal bleeding, and 18 (45%) with increased fecal urgency. Overall, 13 (65%) patients with positive GI PCR were treated with antibiotics, compared to 12 (30%) with negative GI PCR, OR 4.3, p=0.01 (Table 1). Positive GI PCR was not associated with symptom recurrence, hospitalization or sepsis or intensive care unit admission within 3 months, or repeat surgery due to pouchitis.
Discussion: The yield of GI PCR for bacterial pathogens in patients with IPAA was low at 1.8%, similar to a previously reported 1.7% for stool culture in IPAA patients. Although patients with positive GI PCR were significantly more likely to be treated with antibiotics, they did not have differences in positive or negative clinical outcomes studied. Further studies should investigate the utility of GI PCR in pouchitis management.

Figure: Figure 1. Bacterial infection in pouchitis by multiplex GI PCR.
All patients with positive C. diff on GI PCR had an additional C. diff toxin B PCR that was also positive.
Abbreviations: GI (Gastrointestinal), PCR (Polymerase chain reaction), C. difficile (Clostridioides difficile), Y. enterocolitica (Yersinia enterocolitica), EAEC (Enteroaggregative Escherichia coli), EPEC (Enteropathogenic Escherichia coli), ETEC (Enterotoxigenic Escherichia coli), P. shigelloides (Plesiomonas shigelloides)
All patients with positive C. diff on GI PCR had an additional C. diff toxin B PCR that was also positive.
Abbreviations: GI (Gastrointestinal), PCR (Polymerase chain reaction), C. difficile (Clostridioides difficile), Y. enterocolitica (Yersinia enterocolitica), EAEC (Enteroaggregative Escherichia coli), EPEC (Enteropathogenic Escherichia coli), ETEC (Enterotoxigenic Escherichia coli), P. shigelloides (Plesiomonas shigelloides)
Disclosures:
Kate Lee indicated no relevant financial relationships.
Zainab Aziz indicated no relevant financial relationships.
Charu Vyas indicated no relevant financial relationships.
Connor Barrett indicated no relevant financial relationships.
Amy Hembree indicated no relevant financial relationships.
Joshua Gray indicated no relevant financial relationships.
Nathan Suek indicated no relevant financial relationships.
Hueyjong Shih indicated no relevant financial relationships.
Michael Artin indicated no relevant financial relationships.
Priya Sehgal indicated no relevant financial relationships.
Adam Faye: Bristol Myers Squibb – Advisory Committee/Board Member.
Bo Shen: AbbVie – Consultant. Janssen – Consultant. Takeda – Consultant.
Kate E. Lee, MD, MS1, Zainab Aziz, BA, BS2, Charu Vyas, BA2, Connor Barrett, BA2, Amy Hembree, MD2, Joshua Gray, MD1, Nathan Suek, MD2, Hueyjong Shih, MD2, Michael Artin, MD2, Priya Sehgal, MD, MPH, MS2, Adam S. Faye, MD, MS3, Bo Shen, MD, FACG2. P3567 - Impact of Gastrointestinal PCR in Patients With Ileal Pouch-Anal Anastomosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

