Tuesday Poster Session
Category: IBD
P3570 - Safety and Efficacy of Ustekinumab and Vedolizumab Among Older Adults with Inflammatory Bowel Disease
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- MS
Moniyka Sachar, MD
NYU Langone Health
New York, New York
Presenting Author(s)
Moniyka Sachar, MD1, Cristina Fernandez, MD, MPH1, William Beaty, 2, Pakdee Rojanasopondist, MD3, Olivia Delau, MS2, Alice Li, BS4, Megan Murphy, MD5, Jordan Axelrad, MD, MPH2, Simon J. Hong, MD1, Ariela Holmer, MD5, Shannon Chang, MD, MBA1, David Hudesman, MD6, Seymour Katz, MD6, Lisa Malter, MD2, Adam S. Faye, MD, MS7
1NYU Langone Health, New York, NY; 2NYU Grossman School of Medicine, New York, NY; 3University of Washington, Seattle, WA; 4NYU School of Public Health, New York, NY; 5NYU Langone, New York, NY; 6NYU, New York, NY; 7New York University Langone Health, New York, NY
Introduction: There is a lack of safety and efficacy data for newer biologic agents among adults 60 years old with inflammatory bowel disease (IBD) given their limited inclusion in clinical trials. We conducted a retrospective cohort study comparing the therapeutic efficacy and adverse events associated with ustekinumab (UST) or vedolizumab (VDZ) use in older adults as compared to younger adults with IBD.
Methods: This single-center retrospective study compared adults 18 to 60 years old to individuals ≥60 years old with a confirmed diagnosis of IBD who began VDZ or UST treatment between 2014-2021. Endoscopic remission was the primary efficacy outcome, with endoscopic response and clinical remission secondary outcomes. The primary safety outcome was infection-related hospitalization, with secondary outcomes including non-severe side-effects. Chi-square, Fisher’s exact tests were used to compare outcomes by age, and multivariate regression to compare all predictors associated with safety and efficacy.
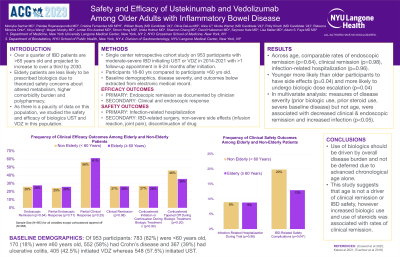
Results: Of 953 participants: 783 (82%) were < 60 years old, 170 (18%) were ≥60 years old, 367 (39%) had ulcerative colitis and 552 (58%) had Crohn’s disease, 405 initiated VDZ whereas 548 initiated UST. Baseline characteristics were similar across age; however, prior treatment with an anti-TNF biologic and/or immunomodulator was more common in younger participants (p< 0.01). When assessing efficacy, younger and older participants had comparable rates of endoscopic remission (25.9% vs 27.7%, p=0.64) and clinical remission (26.6% vs 26.5%, p=0.98) (Figure 1). When assessing safety across age, infection-related hospitalization rates were comparable (8.9% vs 8.8%, p=0.96) and younger participants were more likely than older participants to have non-severe adverse events (19.8% vs 12.8%, p=0.04). Biologic dose escalation was more frequent in younger patients on VDZ than older patients (39% vs 25%; p≤0.05); there was no association between age and other secondary outcomes (Figure 1). In multivariate analysis, measures of disease severity (prior biologic use, prior steroid use, severe baseline disease) but not age, were associated with decreased clinical and endoscopic remission and increased infection risk (p< 0.05) (Table 1).
Discussion: The use of UST and VDZ had similar efficacy and safety outcomes in older adults as compared to younger individuals with IBD. Decisions to utilize these biologics should be driven by overall disease burden, and not be deferred due to advanced chronological age alone.

Disclosures:
Moniyka Sachar, MD1, Cristina Fernandez, MD, MPH1, William Beaty, 2, Pakdee Rojanasopondist, MD3, Olivia Delau, MS2, Alice Li, BS4, Megan Murphy, MD5, Jordan Axelrad, MD, MPH2, Simon J. Hong, MD1, Ariela Holmer, MD5, Shannon Chang, MD, MBA1, David Hudesman, MD6, Seymour Katz, MD6, Lisa Malter, MD2, Adam S. Faye, MD, MS7. P3570 - Safety and Efficacy of Ustekinumab and Vedolizumab Among Older Adults with Inflammatory Bowel Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1NYU Langone Health, New York, NY; 2NYU Grossman School of Medicine, New York, NY; 3University of Washington, Seattle, WA; 4NYU School of Public Health, New York, NY; 5NYU Langone, New York, NY; 6NYU, New York, NY; 7New York University Langone Health, New York, NY
Introduction: There is a lack of safety and efficacy data for newer biologic agents among adults 60 years old with inflammatory bowel disease (IBD) given their limited inclusion in clinical trials. We conducted a retrospective cohort study comparing the therapeutic efficacy and adverse events associated with ustekinumab (UST) or vedolizumab (VDZ) use in older adults as compared to younger adults with IBD.
- Delete highlight and card
- Add a new card to this highlight
- Collect highlight and card
Methods: This single-center retrospective study compared adults 18 to 60 years old to individuals ≥60 years old with a confirmed diagnosis of IBD who began VDZ or UST treatment between 2014-2021. Endoscopic remission was the primary efficacy outcome, with endoscopic response and clinical remission secondary outcomes. The primary safety outcome was infection-related hospitalization, with secondary outcomes including non-severe side-effects. Chi-square, Fisher’s exact tests were used to compare outcomes by age, and multivariate regression to compare all predictors associated with safety and efficacy.
- Delete highlight and card
- Add a new card to this highlight
- Collect highlight and card
Results: Of 953 participants: 783 (82%) were < 60 years old, 170 (18%) were ≥60 years old, 367 (39%) had ulcerative colitis and 552 (58%) had Crohn’s disease, 405 initiated VDZ whereas 548 initiated UST. Baseline characteristics were similar across age; however, prior treatment with an anti-TNF biologic and/or immunomodulator was more common in younger participants (p< 0.01). When assessing efficacy, younger and older participants had comparable rates of endoscopic remission (25.9% vs 27.7%, p=0.64) and clinical remission (26.6% vs 26.5%, p=0.98) (Figure 1). When assessing safety across age, infection-related hospitalization rates were comparable (8.9% vs 8.8%, p=0.96) and younger participants were more likely than older participants to have non-severe adverse events (19.8% vs 12.8%, p=0.04). Biologic dose escalation was more frequent in younger patients on VDZ than older patients (39% vs 25%; p≤0.05); there was no association between age and other secondary outcomes (Figure 1). In multivariate analysis, measures of disease severity (prior biologic use, prior steroid use, severe baseline disease) but not age, were associated with decreased clinical and endoscopic remission and increased infection risk (p< 0.05) (Table 1).
- Delete highlight and card
- Add a new card to this highlight
- Collect highlight and card
Discussion: The use of UST and VDZ had similar efficacy and safety outcomes in older adults as compared to younger individuals with IBD. Decisions to utilize these biologics should be driven by overall disease burden, and not be deferred due to advanced chronological age alone.
- Delete highlight and card
- Add a new card to this highlight
- Collect highlight and card

Figure: Graph 1. Frequency of Efficacy and Safety Outcomes Across Participant Age (N=953)
*P-values calculated via Pearson’s chi-square analysis. Intention to treat (ITT) analysis was used to address missing data.
1: Endoscopic remission defined as clinician documentation of “inactive” colitis on follow-up endoscopy during trial. Partial endoscopic response defined as clinician documentation of improvement in endoscopic score from “moderate-severe or severe” colitis on baseline endoscopy to “mild” or “moderate” colitis on follow-up endoscopy during trial. Endoscopic remission defined as clinician documentation of “inactive” colitis on follow-up endoscopy during trial.
2: Clinical remission defined as clinician report of no IBD-related symptoms in participant. Partial clinical response defined as clinician report of improvement in at least one IBD-related symptom in participant.
3: Non-severe safety outcomes reported by clinicians as secondary to the biologic treatment, including infection or abscess not requiring hospitalization, joint pain or nausea attributed to biologic use, and infusion or injection site reaction.
*P-values calculated via Pearson’s chi-square analysis. Intention to treat (ITT) analysis was used to address missing data.
1: Endoscopic remission defined as clinician documentation of “inactive” colitis on follow-up endoscopy during trial. Partial endoscopic response defined as clinician documentation of improvement in endoscopic score from “moderate-severe or severe” colitis on baseline endoscopy to “mild” or “moderate” colitis on follow-up endoscopy during trial. Endoscopic remission defined as clinician documentation of “inactive” colitis on follow-up endoscopy during trial.
2: Clinical remission defined as clinician report of no IBD-related symptoms in participant. Partial clinical response defined as clinician report of improvement in at least one IBD-related symptom in participant.
3: Non-severe safety outcomes reported by clinicians as secondary to the biologic treatment, including infection or abscess not requiring hospitalization, joint pain or nausea attributed to biologic use, and infusion or injection site reaction.
Disclosures:
Moniyka Sachar indicated no relevant financial relationships.
Cristina Fernandez indicated no relevant financial relationships.
William Beaty indicated no relevant financial relationships.
Pakdee Rojanasopondist indicated no relevant financial relationships.
Olivia Delau indicated no relevant financial relationships.
Alice Li indicated no relevant financial relationships.
Megan Murphy indicated no relevant financial relationships.
Jordan Axelrad: AbbVie – received consulting fees. Adiso – received consulting fees. BioFire Diagnostics – Consultant, Grant/Research Support. Bristol Myers Squibb – received consulting fees. Fresenius Kabi – received consulting fees. Janssen – received consulting fees. Pfizer – received consulting fees.
Simon Hong: Bristol Meyers Squibb – Advisory Committee/Board Member.
Ariela Holmer indicated no relevant financial relationships.
Shannon Chang: Abbvie – Consultant. Bristol Myers Squibb – Consultant. Pfizer – Consultant.
David Hudesman: Abbvie – Consultant. Avalo – Consultant. BMS – Consultant. Fresenius Kabi – Consultant. Janssen – Consultant, Grant/Research Support. Pfizer – Consultant, Grant/Research Support. Prometheus – Consultant. Takeda – Consultant.
Seymour Katz indicated no relevant financial relationships.
Lisa Malter: Abbvie – Advisory Committee/Board Member, Consultant, Grant/Research Support. Bristol Myers Squibb – Advisory Committee/Board Member. Celltrion – Advisory Committee/Board Member. Janssen – Advisory Committee/Board Member, Grant/Research Support. Merck – Advisory Committee/Board Member. Pfizer – Advisory Committee/Board Member, Grant/Research Support. Takeda – Advisory Committee/Board Member, Grant/Research Support.
Adam Faye: Bristol Myers Squibb – Advisory Committee/Board Member.
Moniyka Sachar, MD1, Cristina Fernandez, MD, MPH1, William Beaty, 2, Pakdee Rojanasopondist, MD3, Olivia Delau, MS2, Alice Li, BS4, Megan Murphy, MD5, Jordan Axelrad, MD, MPH2, Simon J. Hong, MD1, Ariela Holmer, MD5, Shannon Chang, MD, MBA1, David Hudesman, MD6, Seymour Katz, MD6, Lisa Malter, MD2, Adam S. Faye, MD, MS7. P3570 - Safety and Efficacy of Ustekinumab and Vedolizumab Among Older Adults with Inflammatory Bowel Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
