Tuesday Poster Session
Category: IBD
P3573 - Impact of Ozanimod on C-Reactive Protein Levels and the Association with OZA Efficacy in Patients With Moderately to Severely Active Ulcerative Colitis: Data From the Phase 3 True North Study
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
- SH
Sarah Harris, PhD
Bristol Myers Squibb
Princeton, New Jersey
Presenting Author(s)
Sarah Harris, PhD1, Rachel Maddux, PhD2, Chun Wu, PhD1, Yanhua Hu, PhD1, AnnKatrin Petersen, MD1, David T. Rubin, MD, FACG3
1Bristol Myers Squibb, Princeton, NJ; 2Bristol Myers Squibb, Princeton, PA; 3University of Chicago Medicine, Inflammatory Bowel Disease Center, Chicago, IL
Introduction: OZA was approved for treatment (tx) of moderately to severely active UC in adults based on TN study results. CRP is a serum indicator of inflammation and prognosis in inflammatory bowel disease.
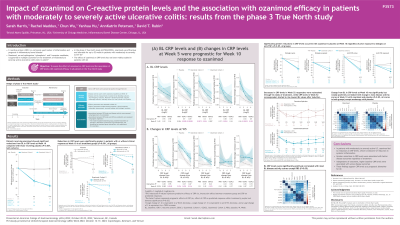
Methods: The effect of OZA on CRP levels and the association of CRP levels with OZA efficacy were assessed in all TN pts. During the 10-wk induction period, pts in Cohort 1 were randomized to OZA 0.92 mg or placebo (PBO) or received open-label OZA 0.92 mg in Cohort 2. OZA clinical responders at Week (W)10 were rerandomized to OZA (OZA/OZA pts) or PBO (PBO/PBO pts) for maintenance through W52. Serum CRP levels were assessed at baseline (BL) through W52. Associations of CRP levels with disease activity (rectal bleeding, stool frequency, Physician’s Global Assessment, and endoscopy subscores and partial and total Mayo scores) and efficacy endpoints (clinical remission, clinical response, endoscopic improvement, mucosal healing, and histologic remission) were assessed using Spearman’s correlation and logistic regression, respectively.
Results: Pts on OZA showed reductions from BL in CRP levels at W10 (P< 0.001 vs PBO); reductions in CRP levels were significantly greater in pts with vs without clinical response at W10 in all tx groups (P< 0.001) (Table). Reductions in CRP levels were maintained through W52; OZA/OZA pts had similar reductions at W52 as OZA/PBO pts; decreases in CRP levels in W52 responders were maintained through W52 of tx, while W52 nonresponder CRP levels started to rise following induction toward BL values (Table). BL CRP levels were significantly positively correlated with most BL disease activity scores (Spearman’s rho 0.2–0.3, P< 0.05) except rectal bleeding subscore. BL CRP levels and change in CRP levels at W5 were prognostic for W10 response. Higher BL CRP levels were associated with lower endoscopic improvement, mucosal healing, and histologic remission at W10 and greater reductions in CRP levels at W5 were associated with better clinical response at W10, independent of tx. Change in CRP levels at W10 was significantly positively correlated with change from BL in most disease activity scores at W10 with OZA and PBO (Spearman’s rho 0.1–0.3, P< 0.05) except endoscopy with PBO.
Discussion: In moderately to severely active UC pts, OZA led to reductions in CRP levels. Higher BL CRP levels were associated with worse disease outcomes. Greater reductions in CRP levels were associated with better disease outcomes regardless of tx, supporting CRP levels as a prognostic biomarker for UC.
Disclosures:
Sarah Harris, PhD1, Rachel Maddux, PhD2, Chun Wu, PhD1, Yanhua Hu, PhD1, AnnKatrin Petersen, MD1, David T. Rubin, MD, FACG3. P3573 - Impact of Ozanimod on C-Reactive Protein Levels and the Association with OZA Efficacy in Patients With Moderately to Severely Active Ulcerative Colitis: Data From the Phase 3 True North Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Bristol Myers Squibb, Princeton, NJ; 2Bristol Myers Squibb, Princeton, PA; 3University of Chicago Medicine, Inflammatory Bowel Disease Center, Chicago, IL
Introduction: OZA was approved for treatment (tx) of moderately to severely active UC in adults based on TN study results. CRP is a serum indicator of inflammation and prognosis in inflammatory bowel disease.
Methods: The effect of OZA on CRP levels and the association of CRP levels with OZA efficacy were assessed in all TN pts. During the 10-wk induction period, pts in Cohort 1 were randomized to OZA 0.92 mg or placebo (PBO) or received open-label OZA 0.92 mg in Cohort 2. OZA clinical responders at Week (W)10 were rerandomized to OZA (OZA/OZA pts) or PBO (PBO/PBO pts) for maintenance through W52. Serum CRP levels were assessed at baseline (BL) through W52. Associations of CRP levels with disease activity (rectal bleeding, stool frequency, Physician’s Global Assessment, and endoscopy subscores and partial and total Mayo scores) and efficacy endpoints (clinical remission, clinical response, endoscopic improvement, mucosal healing, and histologic remission) were assessed using Spearman’s correlation and logistic regression, respectively.
Results: Pts on OZA showed reductions from BL in CRP levels at W10 (P< 0.001 vs PBO); reductions in CRP levels were significantly greater in pts with vs without clinical response at W10 in all tx groups (P< 0.001) (Table). Reductions in CRP levels were maintained through W52; OZA/OZA pts had similar reductions at W52 as OZA/PBO pts; decreases in CRP levels in W52 responders were maintained through W52 of tx, while W52 nonresponder CRP levels started to rise following induction toward BL values (Table). BL CRP levels were significantly positively correlated with most BL disease activity scores (Spearman’s rho 0.2–0.3, P< 0.05) except rectal bleeding subscore. BL CRP levels and change in CRP levels at W5 were prognostic for W10 response. Higher BL CRP levels were associated with lower endoscopic improvement, mucosal healing, and histologic remission at W10 and greater reductions in CRP levels at W5 were associated with better clinical response at W10, independent of tx. Change in CRP levels at W10 was significantly positively correlated with change from BL in most disease activity scores at W10 with OZA and PBO (Spearman’s rho 0.1–0.3, P< 0.05) except endoscopy with PBO.
Discussion: In moderately to severely active UC pts, OZA led to reductions in CRP levels. Higher BL CRP levels were associated with worse disease outcomes. Greater reductions in CRP levels were associated with better disease outcomes regardless of tx, supporting CRP levels as a prognostic biomarker for UC.
Disclosures:
Sarah Harris: Bristol Myers Squibb – employee and/or shareholder.
Rachel Maddux: Bristol Myers Squibb – employee and/or shareholder.
Chun Wu: Bristol Myers Squibb – employee and/or shareholder.
Yanhua Hu: Bristol Myers Squibb – employee and/or shareholder.
AnnKatrin Petersen: Bristol Myers Squibb – employee and/or shareholder.
David T. Rubin: AbbVie – Consultant. Alike Health – Stock Options. AltruBio – Consultant, Stock Options. Aslan Pharmaceuticals – Consultant. Athos Therapeutics – Consultant. Bellatrix Pharmaceuticals – Consultant. Boehringer Ingelheim – Consultant. Bristol Myers Squibb – Consultant. Celgene – Consultant. Chronicles – Consultant. ClostraBio – Consultant. Connect BioPharma – Consultant. Cornerstones Health, Inc – Advisory Committee/Board Member. Crohn's & Colitis Foundation – Advisory Committee/Board Member. Datos Health – Stock Options. EcoR1 – Consultant. Eli Lilly – Consultant. GastroIntestinal Research Foundation – Grant/Research Support. Genentech/Roche – Consultant. Gilead Sciences – Consultant. Helmsley Charitable Trust – Grant/Research Support. Iterative Health – Consultant. Iterative Health – Stock Options. Janssen – Consultant. Kaleido Biosciences – Consultant. Pfizer – Consultant. Prometheus Biosciences – Consultant. Reistone – Consultant. Seres Therapeutics – Consultant. Syneos – Consultant. Takeda – Consultant, Grant/Research Support. Target RWE – Consultant. Trellus Health – Consultant.
Sarah Harris, PhD1, Rachel Maddux, PhD2, Chun Wu, PhD1, Yanhua Hu, PhD1, AnnKatrin Petersen, MD1, David T. Rubin, MD, FACG3. P3573 - Impact of Ozanimod on C-Reactive Protein Levels and the Association with OZA Efficacy in Patients With Moderately to Severely Active Ulcerative Colitis: Data From the Phase 3 True North Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
