Tuesday Poster Session
Category: IBD
P3574 - Link Between Ulcerative Colitis and Augmented Risk of GERD and Associated Complications: A Nationwide Inpatient-based Study
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
.jpeg.jpg)
Xiaoliang Wang, MD, PhD
Marshall University School of Medicine
Huntington, WV
Presenting Author(s)
Xiaoliang Wang, MD, PhD1, Jiayan Wang, MD, PhD1, Zachary Wright, BS1, Gengqing Song, MD2
1Marshall University School of Medicine, Huntington, WV; 2MetroHealth Medical Center, Case Western Reserve University, Cleveland, OH
Introduction: Despite patients often report heartburn and regurgitation in ulcerative colitis (UC), the scientific understanding of its association with gastroesophageal reflux disease (GERD) and related complications like esophageal stricture and Barrett's esophagus is limited. This study aimed to investigate the prevalence and associated risk of GERD and its complications in the UC population.
Methods: The study utilized data from the National Inpatient Sample (NIS), consisting of 7,159,694 patients. We compared GERD patients with and without UC against individuals without GERD, controlling for factors including age, obesity, smoking, hiatal hernia, race, and sex. In addition, UC was evaluated based on the extent of colonic involvement and the presence of esophageal complications. We employed bivariate analyses with the chi-squared test or Fisher exact test (2-tailed) to discern differences among the groups.
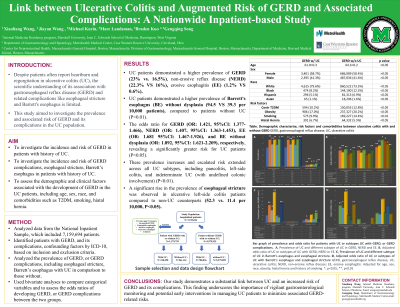
Results: UC patients demonstrated a higher prevalence of GERD (23% vs. 16.5%), non-erosive reflux disease (NERD) (22.3% VS 16%), erosive esophagitis (EE) (1.2% VS 0.6%), Barrett's esophagus (BE) without dysplasia (94.5 VS 39.3 per 10,000 patients), compared to patients without UC (P< 0.01). The odds ratio for GERD, NERD, EE, and BE without dysplasia were 1.421 (95%CI: 1.377-1.466) , 1.407 (95%CI: 1.363-1.453), 1.681 (95%CI: 1.467-1.926), and 1.892 (95%CI: 1.621-2.209), respectively, revealing a significantly greater risk for UC patients (P< 0.05). These prevalence increases and escalated risk extended across all UC subtypes, including pancolitis, left-side colitis, and indeterminate UC (with undefined colonic involvement) (P< 0.01). However, the prevalence and risk of BE with dysplasia remained unchanged. Notably, a significant rise in the prevalence of esophageal stricture was observed in ulcerative left-side colitis patients compared to non-UC counterparts (52.3 vs. 11.4 per 10,000, P< 0.05).
Discussion: Our study demonstrates a substantial link between UC and an increased risk of GERD and its complications. This finding underscores the importance of vigilant gastroenterological monitoring and potential early interventions in managing UC patients to minimize associated GERD-related risks.

Disclosures:
Xiaoliang Wang, MD, PhD1, Jiayan Wang, MD, PhD1, Zachary Wright, BS1, Gengqing Song, MD2. P3574 - Link Between Ulcerative Colitis and Augmented Risk of GERD and Associated Complications: A Nationwide Inpatient-based Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Marshall University School of Medicine, Huntington, WV; 2MetroHealth Medical Center, Case Western Reserve University, Cleveland, OH
Introduction: Despite patients often report heartburn and regurgitation in ulcerative colitis (UC), the scientific understanding of its association with gastroesophageal reflux disease (GERD) and related complications like esophageal stricture and Barrett's esophagus is limited. This study aimed to investigate the prevalence and associated risk of GERD and its complications in the UC population.
Methods: The study utilized data from the National Inpatient Sample (NIS), consisting of 7,159,694 patients. We compared GERD patients with and without UC against individuals without GERD, controlling for factors including age, obesity, smoking, hiatal hernia, race, and sex. In addition, UC was evaluated based on the extent of colonic involvement and the presence of esophageal complications. We employed bivariate analyses with the chi-squared test or Fisher exact test (2-tailed) to discern differences among the groups.
Results: UC patients demonstrated a higher prevalence of GERD (23% vs. 16.5%), non-erosive reflux disease (NERD) (22.3% VS 16%), erosive esophagitis (EE) (1.2% VS 0.6%), Barrett's esophagus (BE) without dysplasia (94.5 VS 39.3 per 10,000 patients), compared to patients without UC (P< 0.01). The odds ratio for GERD, NERD, EE, and BE without dysplasia were 1.421 (95%CI: 1.377-1.466) , 1.407 (95%CI: 1.363-1.453), 1.681 (95%CI: 1.467-1.926), and 1.892 (95%CI: 1.621-2.209), respectively, revealing a significantly greater risk for UC patients (P< 0.05). These prevalence increases and escalated risk extended across all UC subtypes, including pancolitis, left-side colitis, and indeterminate UC (with undefined colonic involvement) (P< 0.01). However, the prevalence and risk of BE with dysplasia remained unchanged. Notably, a significant rise in the prevalence of esophageal stricture was observed in ulcerative left-side colitis patients compared to non-UC counterparts (52.3 vs. 11.4 per 10,000, P< 0.05).
Discussion: Our study demonstrates a substantial link between UC and an increased risk of GERD and its complications. This finding underscores the importance of vigilant gastroenterological monitoring and potential early interventions in managing UC patients to minimize associated GERD-related risks.

Figure: Figure A, Demographic characterize, risk factors and comorbidities between UC with and without GERD. B, Prevalence and odds ratio of GERD and GERD subtypes in patients with all types of UC. C, Prevalence and odds ratio of GERD complications in patients with all types of UC. D, Bar graph of prevalence and odds ratio of GERD and GERD Complications in patients with All type of UC. GERD, gastroesophageal reflux disease; UC, ulcerative colitis, UCPAN, ulcerative pancolitis; UCRPOC, ulcerative proctitis; UCRESCSIG, ulcerative rectosigmoiditis; UCLEFT, left-side colitis; UCOTHER, indetermined UC; OR, odds ratio *, p<0.05; **, p<0.01
Disclosures:
Xiaoliang Wang indicated no relevant financial relationships.
Jiayan Wang indicated no relevant financial relationships.
Zachary Wright indicated no relevant financial relationships.
Gengqing Song indicated no relevant financial relationships.
Xiaoliang Wang, MD, PhD1, Jiayan Wang, MD, PhD1, Zachary Wright, BS1, Gengqing Song, MD2. P3574 - Link Between Ulcerative Colitis and Augmented Risk of GERD and Associated Complications: A Nationwide Inpatient-based Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
