Tuesday Poster Session
Category: IBD
P3579 - Effectiveness of Upadacitinib for Inflammatory Bowel Disease Patients With Pouchitis: Prospective Real-World Experience
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Noa Krugliak Cleveland, MD
University of Chicago Medicine, Inflammatory Bowel Disease Center
Chicago, IL
Presenting Author(s)
Noa Krugliak Cleveland, MD1, Natalie Choi, BA1, David K.. Choi, PharmD1, Sushila Dalal, MD1, David T. Rubin, MD2
1University of Chicago Medicine, Inflammatory Bowel Disease Center, Chicago, IL; 2Inflammatory Bowel Disease Center, University of Chicago Medicine, Chicago, IL
Introduction:
Pouchitis occurs in up to 80% of patients within 2 years of ileal pouch-anal anastomosis (IPAA). Upadacitinib (UPA) is a novel, selective Janus kinase-1 inhibitor that has received regulatory approval for moderately to severely active ulcerative colitis (UC) and Crohn’s disease (CD). However, the effectiveness and safety of UPA therapy for patients with pouchitis is not known. Here we present our real-world experience with UPA in patients with antibiotic-resistant pouchitis.
Methods:
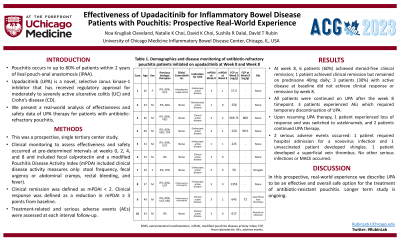
We performed a prospective, real-world analysis of clinical outcomes for patients with IPAA who had antibiotic-resistant pouchitis and were treated with UPA. Clinical monitoring to assess effectiveness and safety occurred at pre-determined intervals at weeks 0, 2, 4, and 8 and included fecal calprotectin and a modified Pouchitis Disease Activity Index (mPDAI included clinical disease activity measures only: stool frequency, fecal urgency or abdominal cramps, rectal bleeding, and fever). Clinical remission was defined as mPDAI < 2. Clinical response was defined as a reduction in mPDAI ≥ 3 points from baseline. Treatment- related and serious adverse events (AEs) were assessed for at each interval follow-up.
Results:
10 patients with antibiotic-resistant IPAA received UPA 45 mg/d. 5 patients were treated with UPA for endoscopically active disease and 5 were treated for clinically and/or biochemically active disease (Table 1). 2 patients were in clinical remission at the time of UPA initiation. By week 8, 6 patients (60%) achieved steroid-free clinical remission; 1 patient achieved clinical remission but remained on prednisone 40mg daily; 3 patients (30%) with active disease at baseline did not achieve clinical response or remission by week 8. All patients were continued on UPA after the week 8 timepoint. 3 patients experienced AEs which required temporary discontinuation of UPA. Upon resuming UPA therapy, 1 patient experienced loss of response and was switched to ustekinumab, and 2 patients continued UPA therapy. There were 2 serious adverse events: 1 patient required hospital admission for a novovirus infection and 1 unvaccinated patient developed shingles. 1 patient developed a superficial vein thrombus. No other serious infections or MACE occurred.
Discussion:
In this prospective, real-world experience we describe UPA to be an effective and overall safe option for the treatment of antibiotic-resistant pouchitis. Longer term study is ongoing.
Disclosures:
Noa Krugliak Cleveland, MD1, Natalie Choi, BA1, David K.. Choi, PharmD1, Sushila Dalal, MD1, David T. Rubin, MD2. P3579 - Effectiveness of Upadacitinib for Inflammatory Bowel Disease Patients With Pouchitis: Prospective Real-World Experience, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Chicago Medicine, Inflammatory Bowel Disease Center, Chicago, IL; 2Inflammatory Bowel Disease Center, University of Chicago Medicine, Chicago, IL
Introduction:
Pouchitis occurs in up to 80% of patients within 2 years of ileal pouch-anal anastomosis (IPAA). Upadacitinib (UPA) is a novel, selective Janus kinase-1 inhibitor that has received regulatory approval for moderately to severely active ulcerative colitis (UC) and Crohn’s disease (CD). However, the effectiveness and safety of UPA therapy for patients with pouchitis is not known. Here we present our real-world experience with UPA in patients with antibiotic-resistant pouchitis.
Methods:
We performed a prospective, real-world analysis of clinical outcomes for patients with IPAA who had antibiotic-resistant pouchitis and were treated with UPA. Clinical monitoring to assess effectiveness and safety occurred at pre-determined intervals at weeks 0, 2, 4, and 8 and included fecal calprotectin and a modified Pouchitis Disease Activity Index (mPDAI included clinical disease activity measures only: stool frequency, fecal urgency or abdominal cramps, rectal bleeding, and fever). Clinical remission was defined as mPDAI < 2. Clinical response was defined as a reduction in mPDAI ≥ 3 points from baseline. Treatment- related and serious adverse events (AEs) were assessed for at each interval follow-up.
Results:
10 patients with antibiotic-resistant IPAA received UPA 45 mg/d. 5 patients were treated with UPA for endoscopically active disease and 5 were treated for clinically and/or biochemically active disease (Table 1). 2 patients were in clinical remission at the time of UPA initiation. By week 8, 6 patients (60%) achieved steroid-free clinical remission; 1 patient achieved clinical remission but remained on prednisone 40mg daily; 3 patients (30%) with active disease at baseline did not achieve clinical response or remission by week 8. All patients were continued on UPA after the week 8 timepoint. 3 patients experienced AEs which required temporary discontinuation of UPA. Upon resuming UPA therapy, 1 patient experienced loss of response and was switched to ustekinumab, and 2 patients continued UPA therapy. There were 2 serious adverse events: 1 patient required hospital admission for a novovirus infection and 1 unvaccinated patient developed shingles. 1 patient developed a superficial vein thrombus. No other serious infections or MACE occurred.
Discussion:
In this prospective, real-world experience we describe UPA to be an effective and overall safe option for the treatment of antibiotic-resistant pouchitis. Longer term study is ongoing.
Disclosures:
Noa Krugliak Cleveland: Bristol Meyer Squibb – Speakers Bureau. Neurologica – Consultant. Takeda – Consultant.
Natalie Choi indicated no relevant financial relationships.
David Choi: Abbvie – Consultant. Boehringer Ingelheim – Consultant. Bristol Myers Squibb – Consultant. Janssen Pharmaceuticals – Consultant, Speakers Bureau. Prometheus Laboratory – Consultant.
Sushila Dalal: AbbVie – Consultant, Speakers Bureau. Pfizer – Consultant, Speakers Bureau.
David Rubin: AbbVie – Consultant, personal fees. AltruBio – Consultant, personal fees. Aslan Pharmaceuticals – Consultant. Athos Therapeutics – Consultant. Bellatrix Pharmaceuticals – Consultant. Boehringer Ingelheim – Consultant, personal fees. Bristol Myers Squibb – Consultant. Celgene Chronicles – Consultant. ClostraBio – Consultant. Connect BioPharma – Consultant. Corp/Syneos – Consultant. Eco R1 – Consultant. GastroIntestinal Research Foundation – Grant/Research Support. Genentech/Roche – Consultant. Gilead Sciences – Consultant, personal fees. Helmsley Charitable Trust – Grant/Research Support. Iterative Health – Consultant. Janssen Pharmaceuticals – Consultant, personal fees. Kaleido Biosciences – Consultant. Lilly – Consultant. Pfizer – Consultant, personal fees. Prometheus Biosciences – Consultant. Reistone Biopharma – Consultant, personal fees. Seres Therapeutics – Consultant. Takeda – Consultant, Grant/Research Support, Personal fees. Target RWE – Consultant. Trellus Health – Consultant.
Noa Krugliak Cleveland, MD1, Natalie Choi, BA1, David K.. Choi, PharmD1, Sushila Dalal, MD1, David T. Rubin, MD2. P3579 - Effectiveness of Upadacitinib for Inflammatory Bowel Disease Patients With Pouchitis: Prospective Real-World Experience, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
