Tuesday Poster Session
Category: IBD
P3585 - Prevalence of Cardiac Conduction Disorders of Interest Among Adults With and Without Moderately to Severely Active Ulcerative Colitis in the United States: A Real-World Analysis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- PD
Parakkal Deepak, MBBS, MS
Washington University in St. Louis School of Medicine
SAINT LOUIS, MO
Presenting Author(s)
Parakkal Deepak, MBBS, MS1, Damemarie Paul, MPH2, Shweta Shah, PhD3, Ching An Wang, MA4, Ye Wang, PhD3, Matthew Cato, MPH5, Tomas G. Neilan, MD6, Garrett Lawlor, MD3
1Washington University in St. Louis School of Medicine, St. Louis, MO; 2BMS, Summit, NJ; 3Bristol Myers Squibb, Princeton, NJ; 4Bristol Myers Squibb, Lawrenceville, NJ; 5BMS, New York, NY; 6Harvard Medical School, Boston, MA
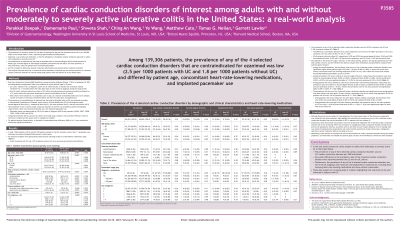
Introduction: Patients (pts) with select cardiac conduction disorders (CCDs) identified via electrocardiogram are contraindicated for ozanimod use. Claims data were used to estimate and compare the real-world prevalence of 4 CCDs among pts with and without (w/o) ulcerative colitis (UC).
Methods: MarketScan Commercial claims data (10/2016-09/2021) were used to identify adults with ≥2 and w/o UC diagnostic claims (index date: date imputed for non-UC cohort). Prevalence rates of 4 CCDs were identified by ICD-10-CM diagnosis codes: second-degree atrioventricular (AV) block (I44.1), complete AV block (I44.2), sick sinus syndrome (SSS; I49.5), or sinoatrial (SA) block (I45.5). Pts with and w/o UC were matched on age, sex, Charlson comorbidity index score category, number of months of continuous enrollment before and after index date, and hypertension by 1:1 propensity score matching (PSM). Prevalence rates from pairwise comparison (P < 0.05) were stratified by age, use of heart rate–lowering medications (antiarrhythmic, beta blockers, calcium channel blockers, and ivabradine), or presence of a pacemaker.
Results: After PSM, 69,653 pts were included in each group. The groups were similar; overall, 52.3% were female and mean age was ~46 years. Antiarrhythmics were used by 9.96% of UC pts and 4.91% of non-UC pts. Rates of CCDs were higher in pts aged ≥50 (0.40%) vs < 50 (0.09%) years, in those using (0.70%) vs not using (0.11%) heart rate–lowering medications, and in those with (27.27%) vs w/o pacemakers (0.10%). In the UC and non-UC groups, rates of CCDs were low (0.25% and 0.18%, respectively). In the UC and non-UC groups, rates of second-degree AV block, complete AV block, and SA block were similar but rates of SSS were not (UC: 0.18% vs non-UC: 0.12%). There were no differences in rates of second-degree AV block, complete AV block, or SA block for UC vs non-UC pts w/o heart rate–lowering medications but rates of SSS were different (UC: 0.09% and non-UC: 0.05%). For UC vs non-UC pts w/o a pacemaker, rates of SA block and SSS were different (UC: 0.01% and 0.09%; non-UC: < 0.01% and 0.05%, respectively), whereas second-degree AV block and complete AV block were similar. The same trend was observed between the 2 groups for pts aged ≥50 years w/o a pacemaker.
Discussion: Prevalence of CCDs of interest was low and differed by pt age, concomitant cardiac medications, and pacemaker use. The prevalence of CCDs of interest in pts with UC who would be contraindicated for ozanimod were generally similar to pts w/o UC.
Disclosures:
Parakkal Deepak, MBBS, MS1, Damemarie Paul, MPH2, Shweta Shah, PhD3, Ching An Wang, MA4, Ye Wang, PhD3, Matthew Cato, MPH5, Tomas G. Neilan, MD6, Garrett Lawlor, MD3. P3585 - Prevalence of Cardiac Conduction Disorders of Interest Among Adults With and Without Moderately to Severely Active Ulcerative Colitis in the United States: A Real-World Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Washington University in St. Louis School of Medicine, St. Louis, MO; 2BMS, Summit, NJ; 3Bristol Myers Squibb, Princeton, NJ; 4Bristol Myers Squibb, Lawrenceville, NJ; 5BMS, New York, NY; 6Harvard Medical School, Boston, MA
Introduction: Patients (pts) with select cardiac conduction disorders (CCDs) identified via electrocardiogram are contraindicated for ozanimod use. Claims data were used to estimate and compare the real-world prevalence of 4 CCDs among pts with and without (w/o) ulcerative colitis (UC).
Methods: MarketScan Commercial claims data (10/2016-09/2021) were used to identify adults with ≥2 and w/o UC diagnostic claims (index date: date imputed for non-UC cohort). Prevalence rates of 4 CCDs were identified by ICD-10-CM diagnosis codes: second-degree atrioventricular (AV) block (I44.1), complete AV block (I44.2), sick sinus syndrome (SSS; I49.5), or sinoatrial (SA) block (I45.5). Pts with and w/o UC were matched on age, sex, Charlson comorbidity index score category, number of months of continuous enrollment before and after index date, and hypertension by 1:1 propensity score matching (PSM). Prevalence rates from pairwise comparison (P < 0.05) were stratified by age, use of heart rate–lowering medications (antiarrhythmic, beta blockers, calcium channel blockers, and ivabradine), or presence of a pacemaker.
Results: After PSM, 69,653 pts were included in each group. The groups were similar; overall, 52.3% were female and mean age was ~46 years. Antiarrhythmics were used by 9.96% of UC pts and 4.91% of non-UC pts. Rates of CCDs were higher in pts aged ≥50 (0.40%) vs < 50 (0.09%) years, in those using (0.70%) vs not using (0.11%) heart rate–lowering medications, and in those with (27.27%) vs w/o pacemakers (0.10%). In the UC and non-UC groups, rates of CCDs were low (0.25% and 0.18%, respectively). In the UC and non-UC groups, rates of second-degree AV block, complete AV block, and SA block were similar but rates of SSS were not (UC: 0.18% vs non-UC: 0.12%). There were no differences in rates of second-degree AV block, complete AV block, or SA block for UC vs non-UC pts w/o heart rate–lowering medications but rates of SSS were different (UC: 0.09% and non-UC: 0.05%). For UC vs non-UC pts w/o a pacemaker, rates of SA block and SSS were different (UC: 0.01% and 0.09%; non-UC: < 0.01% and 0.05%, respectively), whereas second-degree AV block and complete AV block were similar. The same trend was observed between the 2 groups for pts aged ≥50 years w/o a pacemaker.
Discussion: Prevalence of CCDs of interest was low and differed by pt age, concomitant cardiac medications, and pacemaker use. The prevalence of CCDs of interest in pts with UC who would be contraindicated for ozanimod were generally similar to pts w/o UC.
Disclosures:
Parakkal Deepak: Abbvie – Advisory Committee/Board Member. BMS – Advisory Committee/Board Member. Boehringer Ingelheim – Grant/Research Support. Fresenius Kabi – Consultant. Janssen – Grant/Research Support. Pfizer/Arena Pharmaceuticals – Grant/Research Support. Prometheus Biosciences – Grant/Research Support. Prometheus Labs – Grant/Research Support. Roche – Grant/Research Support, PI on a study. Sandoz – Advisory Committee/Board Member. Takeda – Grant/Research Support.
Damemarie Paul: BMS – Employee.
Shweta Shah: Bristol Myers Squibb – Employee.
Ching An Wang: Bristol Myers Squibb – Employee.
Ye Wang: Bristol Myers Squibb – Employee, Stock Options.
Matthew Cato: Bristol Myers Squibb – Consultant, Employee.
Tomas G. Neilan: Abbvie – Consultant. AstraZeneca – Grant/Research Support. BMS – Consultant. BMS – Grant/Research Support. CardiolRx – Consultant. Genentech – Consultant. Roche – Consultant. Sanofi – Consultant.
Garrett Lawlor: Bristol Myers Squibb – employee and/or shareholder.
Parakkal Deepak, MBBS, MS1, Damemarie Paul, MPH2, Shweta Shah, PhD3, Ching An Wang, MA4, Ye Wang, PhD3, Matthew Cato, MPH5, Tomas G. Neilan, MD6, Garrett Lawlor, MD3. P3585 - Prevalence of Cardiac Conduction Disorders of Interest Among Adults With and Without Moderately to Severely Active Ulcerative Colitis in the United States: A Real-World Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
