Tuesday Poster Session
Category: IBD
P3587 - Inflammatory Bowel Disease Mortality Is Associated with State-Level Health Disparity in the United States
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Manasik Abdu, MD
University at Buffalo-Catholic Health System
Buffalo, NY
Presenting Author(s)
Manasik Abdu, MD1, Brian M. Quigley, PhD2, Ben Cohen, MD, MAS3
1University at Buffalo-Catholic Health System, Buffalo, NY; 2University at Buffalo, Buffalo, NY; 3Cleveland Clinic, Cleveland, OH
Introduction: In the US, Inflammatory Bowel Disease (IBD) affected 3 million adults (~1.3% of the population) in 2015. IBD-related deaths commonly stem from comorbid conditions and complications. State-level health disparities can impact disease outcomes. This study aims to examine their association with IBD-related mortality and identify factors impacting IBD outcomes at a state level.
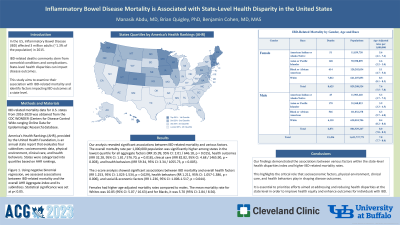
Methods: IBD-related mortality data for U.S. states from 2016-2020 was obtained from the CDC WONDER (Centers for Disease Control Wide-ranging Online Data for Epidemiologic Research) database. America’s Health Rankings (AHR), provided by the United Health Foundation, is an annual state report that evaluates four subindices: socioeconomic data, physical environment, clinical care, and health behaviors. States were categorized into quartiles based on AHR rankings, Figure 1. Using negative binomial regression, we assessed associations between IBD-related mortality and the overall AHR Aggregate-index and its subindices. Statistical significance was set at p< 0.05.
Results: Our analysis revealed significant associations between IBD-related mortality and various factors, Table 1.1. The overall mortality rate per 1,000,000 population was significantly higher among states in the lowest quartile for all aggregate factors (IRR 35.99, 95% CI: 2.01 / 646.18, p = 0.015), health outcomes (IRR 32.28, 95% CI: 1.81 / 576.70, p = 0.018), clinical care (IRR 82.82, 95% CI: 4.68 / 1465.90, p = 0.003), and health behaviors (IRR 59.34, 95% CI: 3.34 / 1055.73, p = 0.005). The z-score analysis showed significant associations between IBD mortality and overall health factors (RR 1.253, 95% CI: 1.023-1.534, p = 0.029), health behaviors (RR 1.211, 95% CI: 1.057-1.386, p = 0.006), and social & economic factors (RR 1.236, 95% CI: 1.006-1.517, p = 0.044). Females had higher age-adjusted mortality rates compared to males, Table 1.2. The mean mortality rate for Whites was 10.85 (95% CI: 5.07 / 16.63) and for Blacks, it was 5.70 (95% CI: 2.84 / 8.56).
Discussion: Our findings demonstrated the associations between various factors within the state-level health disparities index and higher IBD-related mortality rates. This highlights the critical role that socioeconomic factors, physical environment, clinical care, and health behaviors play in shaping disease outcomes. It is essential to prioritize efforts aimed at addressing and reducing health disparities at the state level in order to improve health equity and enhance outcomes for individuals with IBD.

Disclosures:
Manasik Abdu, MD1, Brian M. Quigley, PhD2, Ben Cohen, MD, MAS3. P3587 - Inflammatory Bowel Disease Mortality Is Associated with State-Level Health Disparity in the United States, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University at Buffalo-Catholic Health System, Buffalo, NY; 2University at Buffalo, Buffalo, NY; 3Cleveland Clinic, Cleveland, OH
Introduction: In the US, Inflammatory Bowel Disease (IBD) affected 3 million adults (~1.3% of the population) in 2015. IBD-related deaths commonly stem from comorbid conditions and complications. State-level health disparities can impact disease outcomes. This study aims to examine their association with IBD-related mortality and identify factors impacting IBD outcomes at a state level.
Methods: IBD-related mortality data for U.S. states from 2016-2020 was obtained from the CDC WONDER (Centers for Disease Control Wide-ranging Online Data for Epidemiologic Research) database. America’s Health Rankings (AHR), provided by the United Health Foundation, is an annual state report that evaluates four subindices: socioeconomic data, physical environment, clinical care, and health behaviors. States were categorized into quartiles based on AHR rankings, Figure 1. Using negative binomial regression, we assessed associations between IBD-related mortality and the overall AHR Aggregate-index and its subindices. Statistical significance was set at p< 0.05.
Results: Our analysis revealed significant associations between IBD-related mortality and various factors, Table 1.1. The overall mortality rate per 1,000,000 population was significantly higher among states in the lowest quartile for all aggregate factors (IRR 35.99, 95% CI: 2.01 / 646.18, p = 0.015), health outcomes (IRR 32.28, 95% CI: 1.81 / 576.70, p = 0.018), clinical care (IRR 82.82, 95% CI: 4.68 / 1465.90, p = 0.003), and health behaviors (IRR 59.34, 95% CI: 3.34 / 1055.73, p = 0.005). The z-score analysis showed significant associations between IBD mortality and overall health factors (RR 1.253, 95% CI: 1.023-1.534, p = 0.029), health behaviors (RR 1.211, 95% CI: 1.057-1.386, p = 0.006), and social & economic factors (RR 1.236, 95% CI: 1.006-1.517, p = 0.044). Females had higher age-adjusted mortality rates compared to males, Table 1.2. The mean mortality rate for Whites was 10.85 (95% CI: 5.07 / 16.63) and for Blacks, it was 5.70 (95% CI: 2.84 / 8.56).
Discussion: Our findings demonstrated the associations between various factors within the state-level health disparities index and higher IBD-related mortality rates. This highlights the critical role that socioeconomic factors, physical environment, clinical care, and health behaviors play in shaping disease outcomes. It is essential to prioritize efforts aimed at addressing and reducing health disparities at the state level in order to improve health equity and enhance outcomes for individuals with IBD.

Figure: Figure1. States Quartiles by America’s Health Rankings (AHR)
Disclosures:
Manasik Abdu indicated no relevant financial relationships.
Brian Quigley indicated no relevant financial relationships.
Ben Cohen indicated no relevant financial relationships.
Manasik Abdu, MD1, Brian M. Quigley, PhD2, Ben Cohen, MD, MAS3. P3587 - Inflammatory Bowel Disease Mortality Is Associated with State-Level Health Disparity in the United States, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
