Tuesday Poster Session
Category: IBD
P3589 - The Presence of a Dedicated IBD Clinic Social Worker Has a Positive Impact on IBD Patients' Mental Health and Quality of Life
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Jennifer L. Grossman, MD
University of Maryland School of Medicine
Baltimore, MD
Presenting Author(s)
Jennifer L. Grossman, MD1, Samantha Menegas, BS1, Andrew Leopold, MD1, Benjamin Twery, MD1, Lauren Sibel, MS2, Lauren George, MD1
1University of Maryland School of Medicine, Baltimore, MD; 2University of Maryland Medical Center, Baltimore, MD
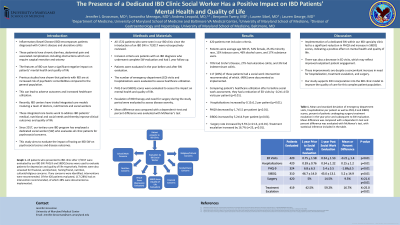
Introduction: Patients with Inflammatory Bowel Disease (IBD) are at increased risk of psychiatric comorbidities compared to the general population. This can lead to adverse outcomes and increased healthcare utilization. Our tertiary care IBD program includes a dedicated social worker (SW) who evaluates all clinic patients for psychosocial concerns to mitigate this effect. This study aims to evaluate the impact of having an IBD SW on psychosocial scores and disease outcomes.
Methods: All 1721 patients who were seen in our IBD clinic since the introduction of an IBD SW in 7/2017 were retrospectively reviewed. Inclusion criteria are patients with an IBD diagnosis who underwent complete SW evaluation and had 1 year follow up. Patients were evaluated in the year before and after SW evaluation. The number of emergency department (ED) visits and hospitalizations were evaluated to assess healthcare utilization. PHQ-9 and SIBDQ scores were evaluated to assess the impact on mental health and quality of life. Escalation of IBD therapy and need for surgery during the study period were evaluated to assess disease severity.
Results: 420 patients met inclusion criteria. Patients were average age 38±15, 54% female, 25.4% minority race, 13% tobacco users, 46% alcohol users, and 17% substance users. 70% had Crohn’s Disease, 27% had ulcerative colitis, and 3% had indeterminant colitis. 117 (28%) of these patients had a social work intervention recommended, of which (48%) were documented as implemented.
Comparing patient’s healthcare utilization after to before social work assessment, they had a reduction of ED visits by -0.2±1.4 ED visits per patient (p< 0.01). Hospitalizations increased by 0.15±1.2 per patient (p=0.01). PHQ-9 decreased by 1.7±5.5 per patient (p< 0.01). SIBDQ increased by 5.2±14.9 per patient (p< 0.01). Surgery rate increased by 9.5% (x=21.6, p< 0.01). Treatment escalation increased by 16.7% (x=25, p< 0.01).
Discussion: Implementation of a dedicated SW within our IBD specialty clinic led to a significant reduction in PHQ-9 and increase in SIBDQ scores, indicating a positive effect on mental health and quality of life. There was also a decrease in ED visits, which may reflect improved outpatient patient engagement. These improvements are despite a concomitant increase in need for hospitalization, treatment escalation, and surgery. Our study supports SW incorporation into the IBD clinic model to improve the quality of care for this complex patient population.
Disclosures:
Jennifer L. Grossman, MD1, Samantha Menegas, BS1, Andrew Leopold, MD1, Benjamin Twery, MD1, Lauren Sibel, MS2, Lauren George, MD1. P3589 - The Presence of a Dedicated IBD Clinic Social Worker Has a Positive Impact on IBD Patients' Mental Health and Quality of Life, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Maryland School of Medicine, Baltimore, MD; 2University of Maryland Medical Center, Baltimore, MD
Introduction: Patients with Inflammatory Bowel Disease (IBD) are at increased risk of psychiatric comorbidities compared to the general population. This can lead to adverse outcomes and increased healthcare utilization. Our tertiary care IBD program includes a dedicated social worker (SW) who evaluates all clinic patients for psychosocial concerns to mitigate this effect. This study aims to evaluate the impact of having an IBD SW on psychosocial scores and disease outcomes.
Methods: All 1721 patients who were seen in our IBD clinic since the introduction of an IBD SW in 7/2017 were retrospectively reviewed. Inclusion criteria are patients with an IBD diagnosis who underwent complete SW evaluation and had 1 year follow up. Patients were evaluated in the year before and after SW evaluation. The number of emergency department (ED) visits and hospitalizations were evaluated to assess healthcare utilization. PHQ-9 and SIBDQ scores were evaluated to assess the impact on mental health and quality of life. Escalation of IBD therapy and need for surgery during the study period were evaluated to assess disease severity.
Results: 420 patients met inclusion criteria. Patients were average age 38±15, 54% female, 25.4% minority race, 13% tobacco users, 46% alcohol users, and 17% substance users. 70% had Crohn’s Disease, 27% had ulcerative colitis, and 3% had indeterminant colitis. 117 (28%) of these patients had a social work intervention recommended, of which (48%) were documented as implemented.
Comparing patient’s healthcare utilization after to before social work assessment, they had a reduction of ED visits by -0.2±1.4 ED visits per patient (p< 0.01). Hospitalizations increased by 0.15±1.2 per patient (p=0.01). PHQ-9 decreased by 1.7±5.5 per patient (p< 0.01). SIBDQ increased by 5.2±14.9 per patient (p< 0.01). Surgery rate increased by 9.5% (x=21.6, p< 0.01). Treatment escalation increased by 16.7% (x=25, p< 0.01).
Discussion: Implementation of a dedicated SW within our IBD specialty clinic led to a significant reduction in PHQ-9 and increase in SIBDQ scores, indicating a positive effect on mental health and quality of life. There was also a decrease in ED visits, which may reflect improved outpatient patient engagement. These improvements are despite a concomitant increase in need for hospitalization, treatment escalation, and surgery. Our study supports SW incorporation into the IBD clinic model to improve the quality of care for this complex patient population.
Disclosures:
Jennifer Grossman indicated no relevant financial relationships.
Samantha Menegas indicated no relevant financial relationships.
Andrew Leopold indicated no relevant financial relationships.
Benjamin Twery indicated no relevant financial relationships.
Lauren Sibel indicated no relevant financial relationships.
Lauren George indicated no relevant financial relationships.
Jennifer L. Grossman, MD1, Samantha Menegas, BS1, Andrew Leopold, MD1, Benjamin Twery, MD1, Lauren Sibel, MS2, Lauren George, MD1. P3589 - The Presence of a Dedicated IBD Clinic Social Worker Has a Positive Impact on IBD Patients' Mental Health and Quality of Life, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
