Tuesday Poster Session
Category: IBD
P3592 - Urgently Hospitalized Inflammatory Bowel Disease Patients During the Pandemic Had Higher Rates of Complications Independent of COVID19 Infection
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall

Rama Nanah, MD
Cleveland Clinic
Cleveland, OH
Presenting Author(s)
Rama Nanah, MD1, M Housam Nanah, MD1, Robana Nanah, MD2, Osama Hamid, MBBS1, Ahmed Eltelbany, MD, MPH1, Faris Hammad, MD3, Yazan Abu Omar, MD1, George Khoudary, MD4, Miguel Regueiro, MD5
1Cleveland Clinic, Cleveland, OH; 2University of Aleppo, Cleveland, OH; 3Case Western Reserve University School of Medicine, Cleveland, OH; 4Georgetown University, Washington, DC; 5Cleveland Clinic Lerner College of Medicine, Case Western Reserve University, Cleveland, OH
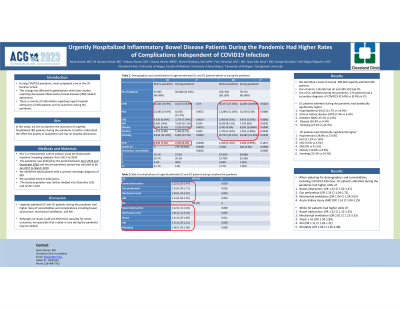
Introduction: During COVID19 pandemic, most outpatient care in the US became virtual. This change has affected hospitalizations with some studies reporting decreased inflammatory bowel diseases (IBD) related admissions. There is scarcity of information regarding urgent hospital admissions of IBD patients and its outcomes during the pandemic. In this study, we aim to examine the outcomes of urgently hospitalized IBD patients during the pandemic to better understand the effect the quality of outpatient care has on hospital admissions.
Methods: this is a retrospective cohort analysis using the Nationwide Inpatient Sampling database from 2017 to 2020. The pandemic was defined by the period between April 2019 and December 2020 and the pre-pandemic period was selected to be Jan 2017 to March 2019. We identified adult patients with a primary discharge diagnosis of IBD. We excluded elective admissions. The study population was further divided into Ulcerative (UC) and Crohn's (CD)
Results: We identified a total of 307,375 urgently admitted IBD patients. Out of which, 118,265 had UC and 189,110 had CD. Out of UC admitted during the pandemic, 270 patients had a secondary diagnosis of COVID19 (0.54%) vs (0.4%) in CD.
UC patients admitted during the pandemic had statistically significantly higher hyperlipidemia (HLD) (21.7% vs 19.9%), chronic kidney disease (CKD) (7.4% vs 6.3%) diabetes (DM) (15.1% vs 14%), Obesity (10.9% vs 9.3%) and smoking (23.3% vs 24.3%) while CD patients had statistically significantly higher hypertension (28.8% vs 27.6%), HLD (11.2% vs 13%), CKD (5.6% vs 4.5%) DM (9% vs 8.11%), Obesity (10.8% vs 8.9%), smoking (23.3% vs 24.3%).
When adjusting for demographics and comorbidities, including COVID19 infection, UC patients admitted during the pandemic had higher odds of bowel obstruction (OR 1.22 CI 1.02-1.47), gut perforation (OR 1.33 CI 1.04-1.71), mechanical ventilation (OR 1.94 CI 1.24-3.03) and acute kidney injury (AKI) (OR 1.14 CI 1.04-1.25) While CD patients had higher odds of bowel obstruction (OR 1.22 CI 1.12-1.33), mechanical ventilation (OR 2.01 CI 1.21-3.33), shock 1.41 (OR 1.05-1.89), AKI (OR 1.11 CI 1.02-1.21) and mortality (OR 1.06 CI 1.05-1.08).
Discussion: Urgently admitted UC and CD patients during the pandemic had higher rates of comorbidities and complications including bowel obstruction, mechanical ventilation, and AKI . Although our study could not determine causality for worse outcomes, we speculate that a delay in care during the pandemic may be related.
Disclosures:
Rama Nanah, MD1, M Housam Nanah, MD1, Robana Nanah, MD2, Osama Hamid, MBBS1, Ahmed Eltelbany, MD, MPH1, Faris Hammad, MD3, Yazan Abu Omar, MD1, George Khoudary, MD4, Miguel Regueiro, MD5. P3592 - Urgently Hospitalized Inflammatory Bowel Disease Patients During the Pandemic Had Higher Rates of Complications Independent of COVID19 Infection, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Cleveland Clinic, Cleveland, OH; 2University of Aleppo, Cleveland, OH; 3Case Western Reserve University School of Medicine, Cleveland, OH; 4Georgetown University, Washington, DC; 5Cleveland Clinic Lerner College of Medicine, Case Western Reserve University, Cleveland, OH
Introduction: During COVID19 pandemic, most outpatient care in the US became virtual. This change has affected hospitalizations with some studies reporting decreased inflammatory bowel diseases (IBD) related admissions. There is scarcity of information regarding urgent hospital admissions of IBD patients and its outcomes during the pandemic. In this study, we aim to examine the outcomes of urgently hospitalized IBD patients during the pandemic to better understand the effect the quality of outpatient care has on hospital admissions.
Methods: this is a retrospective cohort analysis using the Nationwide Inpatient Sampling database from 2017 to 2020. The pandemic was defined by the period between April 2019 and December 2020 and the pre-pandemic period was selected to be Jan 2017 to March 2019. We identified adult patients with a primary discharge diagnosis of IBD. We excluded elective admissions. The study population was further divided into Ulcerative (UC) and Crohn's (CD)
Results: We identified a total of 307,375 urgently admitted IBD patients. Out of which, 118,265 had UC and 189,110 had CD. Out of UC admitted during the pandemic, 270 patients had a secondary diagnosis of COVID19 (0.54%) vs (0.4%) in CD.
UC patients admitted during the pandemic had statistically significantly higher hyperlipidemia (HLD) (21.7% vs 19.9%), chronic kidney disease (CKD) (7.4% vs 6.3%) diabetes (DM) (15.1% vs 14%), Obesity (10.9% vs 9.3%) and smoking (23.3% vs 24.3%) while CD patients had statistically significantly higher hypertension (28.8% vs 27.6%), HLD (11.2% vs 13%), CKD (5.6% vs 4.5%) DM (9% vs 8.11%), Obesity (10.8% vs 8.9%), smoking (23.3% vs 24.3%).
When adjusting for demographics and comorbidities, including COVID19 infection, UC patients admitted during the pandemic had higher odds of bowel obstruction (OR 1.22 CI 1.02-1.47), gut perforation (OR 1.33 CI 1.04-1.71), mechanical ventilation (OR 1.94 CI 1.24-3.03) and acute kidney injury (AKI) (OR 1.14 CI 1.04-1.25) While CD patients had higher odds of bowel obstruction (OR 1.22 CI 1.12-1.33), mechanical ventilation (OR 2.01 CI 1.21-3.33), shock 1.41 (OR 1.05-1.89), AKI (OR 1.11 CI 1.02-1.21) and mortality (OR 1.06 CI 1.05-1.08).
Discussion: Urgently admitted UC and CD patients during the pandemic had higher rates of comorbidities and complications including bowel obstruction, mechanical ventilation, and AKI . Although our study could not determine causality for worse outcomes, we speculate that a delay in care during the pandemic may be related.
Disclosures:
Rama Nanah indicated no relevant financial relationships.
M Housam Nanah indicated no relevant financial relationships.
Robana Nanah indicated no relevant financial relationships.
Osama Hamid indicated no relevant financial relationships.
Ahmed Eltelbany indicated no relevant financial relationships.
Faris Hammad indicated no relevant financial relationships.
Yazan Abu Omar indicated no relevant financial relationships.
George Khoudary indicated no relevant financial relationships.
Miguel Regueiro: AbbVie – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Alfasigma – Advisory Committee/Board Member, Consultant. Allergan – Advisory Committee/Board Member, Consultant. Amgen – Advisory Committee/Board Member, Consultant. Bristol Myers Squibb – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Celgene – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Eli Lilly – Advisory Committee/Board Member, Consultant. Genentech – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Gilead Sciences – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Janssen – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Miraca Labs – Advisory Committee/Board Member, Consultant. Pfizer Inc – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Prometheus – Advisory Committee/Board Member, Consultant. Salix – Advisory Committee/Board Member, Consultant. Seres – Advisory Committee/Board Member, Consultant. Takeda – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Target RWE – Advisory Committee/Board Member, Consultant. UCB – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Wolters Kluwer Health – Royalties.
Rama Nanah, MD1, M Housam Nanah, MD1, Robana Nanah, MD2, Osama Hamid, MBBS1, Ahmed Eltelbany, MD, MPH1, Faris Hammad, MD3, Yazan Abu Omar, MD1, George Khoudary, MD4, Miguel Regueiro, MD5. P3592 - Urgently Hospitalized Inflammatory Bowel Disease Patients During the Pandemic Had Higher Rates of Complications Independent of COVID19 Infection, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
