Tuesday Poster Session
Category: IBD
P3593 - Increased Pulmonary Embolism and Venous Thrombosis in Hospitalized COVID Patients With Inflammatory Bowel Disease: A National Retrospective Cohort Study
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall

Rama Nanah, MD
Cleveland Clinic
Cleveland, OH
Presenting Author(s)
Rama Nanah, MD1, Osama Hamid, MBBS1, Ahmed Eltelbany, MD, MPH1, M Housam Nanah, MD1, Robana Nanah, MD2, Faris Hammad, MD3, George Khoudary, MD4, Miguel Regueiro, MD5
1Cleveland Clinic, Cleveland, OH; 2University of Aleppo, Cleveland, OH; 3Case Western Reserve University School of Medicine, Cleveland, OH; 4Georgetown University, Washington, DC; 5Cleveland Clinic Lerner College of Medicine, Case Western Reserve University, Cleveland, OH
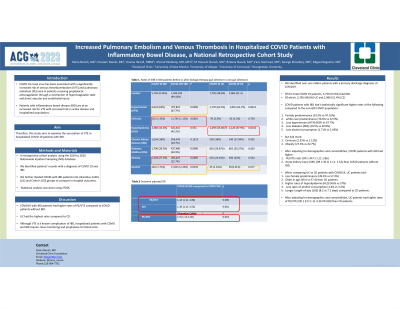
Introduction: COVID 19 novel virus has been associated with a significantly increased risk of venous thromboembolism (VTE) and pulmonary embolism (PE) even in patients receiving prophylactic anticoagulation through a mechanism of hypercoagulable state and direct vascular and endothelial injury. Patients with inflammatory bowel disease (IBD) are at an increased risk for VTE with increased risk in active disease and hospitalized populations. Therefore, this study aims to examine the association of VTE in hospitalized COVID 19 patients with IBD.
Methods: Using the 2019 to 2020 Nationwide Inpatient Sampling (NIS) database. We identified patients’ records with a diagnosis of COVID 19 and IBD. We further divided COVID with IBD patients into Ulcerative Colitis (UC) and Crohn's (CD) groups to compare in-hospital outcomes. Statistical analysis was done using STATA.
Results: We identified over one million patients with a primary discharge diagnosis of COVID19. Of the total COVID 19 patients, 5,750 (0.55%) had IBD. Of which, 2,795 (48.6%) UC and 2,960 (51.4%) CD. COVID patients with IBD had a statistically significant higher female predominance (53.5% vs 47.16%), white race predominance (76.6% vs 52.5%), less HTN (63% vs 67.7%), less diabetes (DM) (29.5% vs 40.9%) and less alcohol consumption (1.71% vs 2.43%) but had more cirrhosis (2.35% vs 1.12%) and obesity (27.3% vs 22.7%) diagnosis compared to the non-IBD COVID population. After adjusting for demographics and comorbidities, COVID patients with IBD had higher PE/VTE rates (OR 1.44 CI 1.11-1.86) and acute kidney injury (AKI) (OR 1.30 CI 1.11-1.52) than COVID patients without IBD.
When comparing UC to CD patients with COVID19. UC patients had less female predominance (49.4% vs 57.4%) and were older in age (49.4 vs 57.4) than CD patients. Additionally, UC patients had higher rates of hyperlipidemia (HLD) (45% vs 37%) but less rates of alcohol consumption (1.6% vs 3.2%). UC patients had longer Length of stay (LOS) (8.2 vs 7.1 days) compared to CD patients. After adjusting for demographics and comorbidities, UC patients had higher rates of PE/VTE (OR 1.9 CI 1.11-3.26 P0.018) than CD patients.
Discussion: COVID19 with IBD patients had higher rates of PE/VTE compared to COVID patients without IBD. UC had the highest rates compared to CD. Although VTE is a known complication of IBD, hospitalized patients with COVID and IBD require close monitoring and prophylaxis for blood clots.
Disclosures:
Rama Nanah, MD1, Osama Hamid, MBBS1, Ahmed Eltelbany, MD, MPH1, M Housam Nanah, MD1, Robana Nanah, MD2, Faris Hammad, MD3, George Khoudary, MD4, Miguel Regueiro, MD5. P3593 - Increased Pulmonary Embolism and Venous Thrombosis in Hospitalized COVID Patients With Inflammatory Bowel Disease: A National Retrospective Cohort Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Cleveland Clinic, Cleveland, OH; 2University of Aleppo, Cleveland, OH; 3Case Western Reserve University School of Medicine, Cleveland, OH; 4Georgetown University, Washington, DC; 5Cleveland Clinic Lerner College of Medicine, Case Western Reserve University, Cleveland, OH
Introduction: COVID 19 novel virus has been associated with a significantly increased risk of venous thromboembolism (VTE) and pulmonary embolism (PE) even in patients receiving prophylactic anticoagulation through a mechanism of hypercoagulable state and direct vascular and endothelial injury. Patients with inflammatory bowel disease (IBD) are at an increased risk for VTE with increased risk in active disease and hospitalized populations. Therefore, this study aims to examine the association of VTE in hospitalized COVID 19 patients with IBD.
Methods: Using the 2019 to 2020 Nationwide Inpatient Sampling (NIS) database. We identified patients’ records with a diagnosis of COVID 19 and IBD. We further divided COVID with IBD patients into Ulcerative Colitis (UC) and Crohn's (CD) groups to compare in-hospital outcomes. Statistical analysis was done using STATA.
Results: We identified over one million patients with a primary discharge diagnosis of COVID19. Of the total COVID 19 patients, 5,750 (0.55%) had IBD. Of which, 2,795 (48.6%) UC and 2,960 (51.4%) CD. COVID patients with IBD had a statistically significant higher female predominance (53.5% vs 47.16%), white race predominance (76.6% vs 52.5%), less HTN (63% vs 67.7%), less diabetes (DM) (29.5% vs 40.9%) and less alcohol consumption (1.71% vs 2.43%) but had more cirrhosis (2.35% vs 1.12%) and obesity (27.3% vs 22.7%) diagnosis compared to the non-IBD COVID population. After adjusting for demographics and comorbidities, COVID patients with IBD had higher PE/VTE rates (OR 1.44 CI 1.11-1.86) and acute kidney injury (AKI) (OR 1.30 CI 1.11-1.52) than COVID patients without IBD.
When comparing UC to CD patients with COVID19. UC patients had less female predominance (49.4% vs 57.4%) and were older in age (49.4 vs 57.4) than CD patients. Additionally, UC patients had higher rates of hyperlipidemia (HLD) (45% vs 37%) but less rates of alcohol consumption (1.6% vs 3.2%). UC patients had longer Length of stay (LOS) (8.2 vs 7.1 days) compared to CD patients. After adjusting for demographics and comorbidities, UC patients had higher rates of PE/VTE (OR 1.9 CI 1.11-3.26 P0.018) than CD patients.
Discussion: COVID19 with IBD patients had higher rates of PE/VTE compared to COVID patients without IBD. UC had the highest rates compared to CD. Although VTE is a known complication of IBD, hospitalized patients with COVID and IBD require close monitoring and prophylaxis for blood clots.
Disclosures:
Rama Nanah indicated no relevant financial relationships.
Osama Hamid indicated no relevant financial relationships.
Ahmed Eltelbany indicated no relevant financial relationships.
M Housam Nanah indicated no relevant financial relationships.
Robana Nanah indicated no relevant financial relationships.
Faris Hammad indicated no relevant financial relationships.
George Khoudary indicated no relevant financial relationships.
Miguel Regueiro: AbbVie – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Alfasigma – Advisory Committee/Board Member, Consultant. Allergan – Advisory Committee/Board Member, Consultant. Amgen – Advisory Committee/Board Member, Consultant. Bristol Myers Squibb – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Celgene – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Eli Lilly – Advisory Committee/Board Member, Consultant. Genentech – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Gilead Sciences – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Janssen – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Miraca Labs – Advisory Committee/Board Member, Consultant. Pfizer Inc – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Prometheus – Advisory Committee/Board Member, Consultant. Salix – Advisory Committee/Board Member, Consultant. Seres – Advisory Committee/Board Member, Consultant. Takeda – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Target RWE – Advisory Committee/Board Member, Consultant. UCB – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Wolters Kluwer Health – Royalties.
Rama Nanah, MD1, Osama Hamid, MBBS1, Ahmed Eltelbany, MD, MPH1, M Housam Nanah, MD1, Robana Nanah, MD2, Faris Hammad, MD3, George Khoudary, MD4, Miguel Regueiro, MD5. P3593 - Increased Pulmonary Embolism and Venous Thrombosis in Hospitalized COVID Patients With Inflammatory Bowel Disease: A National Retrospective Cohort Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

