Tuesday Poster Session
Category: IBD
P3611 - Evaluating the Predictors of Endoscopic Balloon Dilation Failure, Success, and Surgery Prevention in Crohn's Disease-Related Strictures: A 15-Year Experience at a Tertiary Care Center
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- MI
Meera Iyengar, MD
Indiana University School of Medicine
Indianapolis, IN
Presenting Author(s)
Meera Iyengar, MD1, Brittany Baker, MS, DO1, Mahmoud Rahal, MD1, Azizullah Beran, MD2, Justin Ceh, MD1, Hisham Wehbe, MD1, Monika Fischer, MD, MSc, FACG2, Megan Walker, MD2, Sashidhar Sagi, MD1, Matthew Bohm, DO3
1Indiana University School of Medicine, Indianapolis, IN; 2Indiana University, Indianapolis, IN; 3Indiana University Hospital, Indianapolis, IN
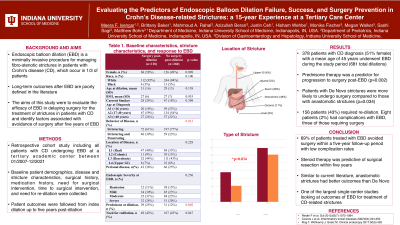
Introduction: Intestinal strictures affect one-third of individuals with Crohn’s disease (CD) within ten years of disease onset. Endoscopic balloon dilation (EBD) is a minimally invasive procedure for managing fibrostenotic strictures in patients with CD. Long-term outcomes after EBD are poorly defined in the literature. The aims of this study are to evaluate the efficacy of EBD in delaying surgery for the treatment of strictures in patients with CD and identify clinical, endoscopic, and stricture-related factors associated with avoidance of surgery after five years of EBD.
Methods: Retrospective cohort study including all patients with CD undergoing EBD at a tertiary academic center between 01/2007-12/2021. Data for demographics, disease characteristics, stricture characteristics, surgical history, medication history, need for surgical intervention, time to surgical intervention, and need for re-dilation were collected. Patient outcomes were followed from their index dilation up to five years post dilation.
Results: 378 patients with CD diagnosis (51% female) with a mean age 45 years underwent EBD during the study period (681 total dilations). The location of the stricture was upper gastrointestinal in 30 patients (9%), ileal (35%), colonic (13%), ileocolonic (44%) in other patients. Among these patients, 118 (31%) required surgery for CD-related stricture during the five-year follow-up periods. Prednisone therapy was a predictor for progression to surgery post-EBD (p=0.002). 156 patients (43%) required re-dilation. Patients with De Novo strictures were more likely to undergo surgery compared to those with anastomotic strictures (p=0.034). Eight patients (2%) had complications with three of those requiring surgery.
Discussion: This is one of the largest single-center studies looking at outcomes of EBD for treatment of CD-related strictures. 69% of patients treated with EBD avoided surgery within a five-year follow-up period. Steroid therapy was predictive of surgical resection within five years. Similar to current literature, anastomotic strictures had better outcomes than De Novo. Larger prospective studies are needed to confirm our results.
Disclosures:
Meera Iyengar, MD1, Brittany Baker, MS, DO1, Mahmoud Rahal, MD1, Azizullah Beran, MD2, Justin Ceh, MD1, Hisham Wehbe, MD1, Monika Fischer, MD, MSc, FACG2, Megan Walker, MD2, Sashidhar Sagi, MD1, Matthew Bohm, DO3. P3611 - Evaluating the Predictors of Endoscopic Balloon Dilation Failure, Success, and Surgery Prevention in Crohn's Disease-Related Strictures: A 15-Year Experience at a Tertiary Care Center, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Indiana University School of Medicine, Indianapolis, IN; 2Indiana University, Indianapolis, IN; 3Indiana University Hospital, Indianapolis, IN
Introduction: Intestinal strictures affect one-third of individuals with Crohn’s disease (CD) within ten years of disease onset. Endoscopic balloon dilation (EBD) is a minimally invasive procedure for managing fibrostenotic strictures in patients with CD. Long-term outcomes after EBD are poorly defined in the literature. The aims of this study are to evaluate the efficacy of EBD in delaying surgery for the treatment of strictures in patients with CD and identify clinical, endoscopic, and stricture-related factors associated with avoidance of surgery after five years of EBD.
Methods: Retrospective cohort study including all patients with CD undergoing EBD at a tertiary academic center between 01/2007-12/2021. Data for demographics, disease characteristics, stricture characteristics, surgical history, medication history, need for surgical intervention, time to surgical intervention, and need for re-dilation were collected. Patient outcomes were followed from their index dilation up to five years post dilation.
Results: 378 patients with CD diagnosis (51% female) with a mean age 45 years underwent EBD during the study period (681 total dilations). The location of the stricture was upper gastrointestinal in 30 patients (9%), ileal (35%), colonic (13%), ileocolonic (44%) in other patients. Among these patients, 118 (31%) required surgery for CD-related stricture during the five-year follow-up periods. Prednisone therapy was a predictor for progression to surgery post-EBD (p=0.002). 156 patients (43%) required re-dilation. Patients with De Novo strictures were more likely to undergo surgery compared to those with anastomotic strictures (p=0.034). Eight patients (2%) had complications with three of those requiring surgery.
Discussion: This is one of the largest single-center studies looking at outcomes of EBD for treatment of CD-related strictures. 69% of patients treated with EBD avoided surgery within a five-year follow-up period. Steroid therapy was predictive of surgical resection within five years. Similar to current literature, anastomotic strictures had better outcomes than De Novo. Larger prospective studies are needed to confirm our results.
Disclosures:
Meera Iyengar indicated no relevant financial relationships.
Brittany Baker indicated no relevant financial relationships.
Mahmoud Rahal indicated no relevant financial relationships.
Azizullah Beran indicated no relevant financial relationships.
Justin Ceh indicated no relevant financial relationships.
Hisham Wehbe indicated no relevant financial relationships.
Monika Fischer: AbbVie – Advisor or Review Panel Member. Bristol Myers Squibb – Advisor or Review Panel Member, Speakers Bureau. Eli Lilly and Company – Advisor or Review Panel Member. Ferring – Advisor or Review Panel Member, DSMB. Janssen – Speakers Bureau. Pfizer – Advisor or Review Panel Member. Rebiotix – DSMB. scioto – Advisor or Review Panel Member. Seres – Advisor or Review Panel Member.
Megan Walker indicated no relevant financial relationships.
Sashidhar Sagi indicated no relevant financial relationships.
Matthew Bohm indicated no relevant financial relationships.
Meera Iyengar, MD1, Brittany Baker, MS, DO1, Mahmoud Rahal, MD1, Azizullah Beran, MD2, Justin Ceh, MD1, Hisham Wehbe, MD1, Monika Fischer, MD, MSc, FACG2, Megan Walker, MD2, Sashidhar Sagi, MD1, Matthew Bohm, DO3. P3611 - Evaluating the Predictors of Endoscopic Balloon Dilation Failure, Success, and Surgery Prevention in Crohn's Disease-Related Strictures: A 15-Year Experience at a Tertiary Care Center, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
