Tuesday Poster Session
Category: IBD
P3633 - Communicating Needs and Features of IBD Experiences (CONFIDE) Survey: Patient and Healthcare Professional Perspectives on Communication Relating to Ulcerative Colitis Symptoms in Canada
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Remo Panaccione, MD
University of Calgary
Calgary, AB, Canada
Presenting Author(s)
Remo Panaccione, MD, FRCPC1, Talat Bessissow, MDCM, MSc, FRCPC2, Jennifer Glass, PhD3, Theresa Hunter Gibble, PhD, MPH4, Christian Atkinson, BSc, MRes5, Marta Braun, PhD3, Hilary Ellis, BA5, Thomas Dewar, BA5, Vipul Jairath, MBChB, DPhil, FRCPC6
1University of Calgary, Calgary, AB, Canada; 2Montreal General Hospital, McGill University Health Center, Montreal, PQ, Canada; 3Eli Lilly Canada, Toronto, ON, Canada; 4Eli Lilly and Company, Indianapolis, IN; 5Adelphi Real World, Bollington, England, United Kingdom; 6Alimentiv and Western University, London, ON, Canada
Introduction: Moderate-to-severe ulcerative colitis (UC) can be associated with impaired quality of life. The Communicating Needs and Features of IBD Experiences (CONFIDE) study aims to increase understanding of patients’ experiences and the impact of IBD on their lives and elucidate any communication gaps between healthcare professionals (HCPs) and patients with moderate-to-severe UC in the United States, Europe, Japan, and Canada. These data focus on Canadian patients and HCPs.
Methods: Online, quantitative, cross-sectional survey was conducted (panel recruitment) between February and April 2023 with patients diagnosed with moderate-to-severe UC and gastroenterologists (GIs) in Canada. Active disease of at least moderate severity defined using criteria based on previous treatment, steroid use, and/or hospitalization. HCPs were GIs responsible for making prescribing decisions for patients with moderate-to-severe UC. Results summarised descriptively.
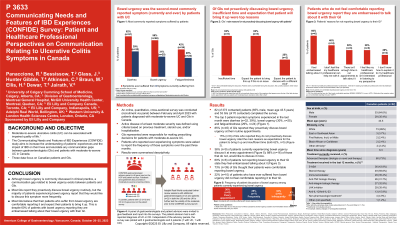
Results: Survey completed by 82 (373 contacted) patients (65% male, mean age 43.5 years (SD 12.6), mean time since diagnosis 6.3 years (SD 7.6, range 1-33 years)) and 53 GIs (70 contacted). The top 3 patient-reported symptoms experienced in the past month were diarrhea (39%, n=32), bowel urgency (BU, 30%, n=25), and fatigue/tiredness (29%, n=24). Among patients currently experiencing BU, 36% (n=9) discussed this at every appointment, of those that did not (n=16), 88% would like to discuss this more. 22% of patients (n=10) who have ever suffered from BU did not feel comfortable reporting BU to their GI. 85% (n=45) GIs reported they proactively discuss BU at routine appointments; 73% (n=39) thought their patients were comfortable reporting BU. GIs who reported that they do not proactively discuss BU (15%, n=8) cited the main reasons as expectation for the patient to bring it up and insufficient time (both 62%, n=5).
Discussion: A communication gap related to BU exists between patients and GIs. Most GIs report they proactively discuss BU routinely, but the majority of patients experiencing this would like to discuss it more. Among GIs that do not routinely proactively discuss BU, most believe their patients are comfortable reporting it. Patients who do not routinely discuss it would like to do so more frequently, but do not feel comfortable reporting it to their GI.
Disclosures:
Remo Panaccione, MD, FRCPC1, Talat Bessissow, MDCM, MSc, FRCPC2, Jennifer Glass, PhD3, Theresa Hunter Gibble, PhD, MPH4, Christian Atkinson, BSc, MRes5, Marta Braun, PhD3, Hilary Ellis, BA5, Thomas Dewar, BA5, Vipul Jairath, MBChB, DPhil, FRCPC6. P3633 - Communicating Needs and Features of IBD Experiences (CONFIDE) Survey: Patient and Healthcare Professional Perspectives on Communication Relating to Ulcerative Colitis Symptoms in Canada, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Calgary, Calgary, AB, Canada; 2Montreal General Hospital, McGill University Health Center, Montreal, PQ, Canada; 3Eli Lilly Canada, Toronto, ON, Canada; 4Eli Lilly and Company, Indianapolis, IN; 5Adelphi Real World, Bollington, England, United Kingdom; 6Alimentiv and Western University, London, ON, Canada
Introduction: Moderate-to-severe ulcerative colitis (UC) can be associated with impaired quality of life. The Communicating Needs and Features of IBD Experiences (CONFIDE) study aims to increase understanding of patients’ experiences and the impact of IBD on their lives and elucidate any communication gaps between healthcare professionals (HCPs) and patients with moderate-to-severe UC in the United States, Europe, Japan, and Canada. These data focus on Canadian patients and HCPs.
Methods: Online, quantitative, cross-sectional survey was conducted (panel recruitment) between February and April 2023 with patients diagnosed with moderate-to-severe UC and gastroenterologists (GIs) in Canada. Active disease of at least moderate severity defined using criteria based on previous treatment, steroid use, and/or hospitalization. HCPs were GIs responsible for making prescribing decisions for patients with moderate-to-severe UC. Results summarised descriptively.
Results: Survey completed by 82 (373 contacted) patients (65% male, mean age 43.5 years (SD 12.6), mean time since diagnosis 6.3 years (SD 7.6, range 1-33 years)) and 53 GIs (70 contacted). The top 3 patient-reported symptoms experienced in the past month were diarrhea (39%, n=32), bowel urgency (BU, 30%, n=25), and fatigue/tiredness (29%, n=24). Among patients currently experiencing BU, 36% (n=9) discussed this at every appointment, of those that did not (n=16), 88% would like to discuss this more. 22% of patients (n=10) who have ever suffered from BU did not feel comfortable reporting BU to their GI. 85% (n=45) GIs reported they proactively discuss BU at routine appointments; 73% (n=39) thought their patients were comfortable reporting BU. GIs who reported that they do not proactively discuss BU (15%, n=8) cited the main reasons as expectation for the patient to bring it up and insufficient time (both 62%, n=5).
Discussion: A communication gap related to BU exists between patients and GIs. Most GIs report they proactively discuss BU routinely, but the majority of patients experiencing this would like to discuss it more. Among GIs that do not routinely proactively discuss BU, most believe their patients are comfortable reporting it. Patients who do not routinely discuss it would like to do so more frequently, but do not feel comfortable reporting it to their GI.
Disclosures:
Remo Panaccione: Abbivax – Consultant. Abbott – Consultant. Abbvie – Advisory Committee/Board Member, Consultant, Speakers Bureau. Alimentiv – Consultant. Amgen – Advisory Committee/Board Member, Consultant, Speakers Bureau. Arena Pharmaceuticals – Advisory Committee/Board Member, Consultant, Speakers Bureau. AstraZeneca – Advisory Committee/Board Member, Consultant. Biogen – Advisory Committee/Board Member, Consultant. Boehringer Ingelheim – Advisory Committee/Board Member, Consultant. Bristol-Myers Squibb – Advisory Committee/Board Member, Consultant, Speakers Bureau. Celgene – Advisory Committee/Board Member, Consultant, Speakers Bureau. Celltrion – Consultant. Cosmos Pharmaceuticals – Consultant. Eisai – Consultant. Elan – Consultant. Eli Lilly – Advisory Committee/Board Member, Consultant, Speakers Bureau. Ferring – Advisory Committee/Board Member, Consultant, Speakers Bureau. Fresenius Kabi – Advisory Committee/Board Member, Speakers Bureau. Galapagos – Consultant. Genentech – Advisory Committee/Board Member. Gilead Sciences – Advisory Committee/Board Member, Consultant, Speakers Bureau. Glaxo-Smith Kline – Advisory Committee/Board Member, Consultant. JAMP Bio – Advisory Committee/Board Member, Consultant. Janssen – Advisory Committee/Board Member, Consultant, Speakers Bureau. Merck – Advisory Committee/Board Member, Consultant, Speakers Bureau. Mylan – Advisory Committee/Board Member, Consultant. Novartis – Advisory Committee/Board Member, Consultant. Oppilan Pharmaceuticals – Advisory Committee/Board Member, Consultant. Organon – Consultant. Pandion Pharma – Advisory Committee/Board Member, Consultant. Pendopharm – Consultant. Pfizer – Advisory Committee/Board Member, Consultant, Speakers Bureau. Progenity – Advisory Committee/Board Member, Consultant. Prometheus Biosciences – Consultant. Protagonist Therapeutics – Advisory Committee/Board Member, Consultant. Roche – Advisory Committee/Board Member, Consultant, Speakers Bureau. Sandoz – Advisory Committee/Board Member, Consultant, Speakers Bureau. Satisfai Health – Consultant. Shire – Advisory Committee/Board Member, Consultant. Sublimity Therapeutics – Advisory Committee/Board Member, Consultant. Takeda – Advisory Committee/Board Member, Consultant, Speakers Bureau. Theravance Biopharma – Consultant. Trellus – Consultant. UCB – Consultant. Ventyx – Advisory Committee/Board Member, Consultant. Viatris – Consultant.
Talat Bessissow: Abbvie – Advisory Committee/Board Member, Consultant, Speakers Bureau. Alimentiv – Consultant. Amgen – Advisory Committee/Board Member, Consultant, Speakers Bureau. Bristol-Myers Squibb – Advisory Committee/Board Member, Consultant, Speakers Bureau. Ferring – Advisory Committee/Board Member, Consultant, Speakers Bureau. Fresenius Kabi – Consultant, Speakers Bureau. Gilead – Consultant, Speakers Bureau. Iterative scope – Consultant, Speakers Bureau. Janssen – Consultant, Speakers Bureau. Merck – Advisory Committee/Board Member, Consultant, Speakers Bureau. Pfizer – Consultant, Speakers Bureau. Roche – Consultant, Speakers Bureau. Sandoz – Consultant, Speakers Bureau. Sanofi – Advisory Committee/Board Member, Consultant, Speakers Bureau. Takeda – Advisory Committee/Board Member, Consultant, Speakers Bureau. Viatris – Consultant, Speakers Bureau.
Jennifer Glass: Eli Lilly – Employee.
Theresa Hunter Gibble: Eli Lilly and Company – Employee, stockholder.
Christian Atkinson: Adelphi Real World – Employee.
Marta Braun: Eli Lilly – Employee.
Hilary Ellis: Adelphi Real World – Employee.
Thomas Dewar: Adelphi Real World – Employee.
Vipul Jairath: Abbvie – Advisory Committee/Board Member, Consultant, Speakers Bureau. Alimentiv – Advisory Committee/Board Member, Consultant. Arena Pharmaceuticals – Advisory Committee/Board Member, Consultant. Asahi Kasei Pharma – Advisory Committee/Board Member, Consultant. Asieris – Advisory Committee/Board Member, Consultant. AstraZeneca – Advisory Committee/Board Member, Consultant. Avoro Capital – Advisory Committee/Board Member, Consultant. Bristol-Myers Squibb – Advisory Committee/Board Member, Consultant, Speakers Bureau. Celltrion – Advisory Committee/Board Member, Consultant. Eli Lilly – Advisory Committee/Board Member, Consultant. EndPoint Health – Advisory Committee/Board Member, Consultant. Enthera – Advisory Committee/Board Member, Consultant. Ferring – Advisory Committee/Board Member, Consultant, Speakers Bureau. Flagship Pioneering – Advisory Committee/Board Member, Consultant. Fresenius Kabi – Advisory Committee/Board Member, Consultant, Speakers Bureau. Galapagos – Advisory Committee/Board Member, Consultant, Speakers Bureau. Genentech – Advisory Committee/Board Member, Consultant. Gilead Sciences – Advisory Committee/Board Member, Consultant. Glaxo-Smith Kline – Advisory Committee/Board Member, Consultant. Glide Healthcare – Advisory Committee/Board Member, Consultant. Innomar – Advisory Committee/Board Member, Consultant. JAMP Bio – Advisory Committee/Board Member, Consultant. Janssen – Advisory Committee/Board Member, Consultant, Speakers Bureau. Merck – Advisory Committee/Board Member, Consultant. Metacrine – Advisory Committee/Board Member, Consultant. Mylan – Advisory Committee/Board Member, Consultant. Pandion Pharma – Advisory Committee/Board Member, Consultant. Pendopharm – Advisory Committee/Board Member, Consultant. Pfizer – Advisory Committee/Board Member, Consultant, Speakers Bureau. Prometheus Biosciences – Advisory Committee/Board Member, Consultant. Protagonist Therapeutics – Advisory Committee/Board Member, Consultant. Reistone Pharma – Advisory Committee/Board Member, Consultant. Roche – Advisory Committee/Board Member, Consultant. Roivant – Advisory Committee/Board Member, Consultant. Sandoz – Advisory Committee/Board Member, Consultant. SCOPE – Advisory Committee/Board Member, Consultant. Second genome – Advisory Committee/Board Member, Consultant. Shire – Speakers Bureau. Sorriso Pharmaceuticals – Advisory Committee/Board Member, Consultant. Takeda – Advisory Committee/Board Member, Consultant, Speakers Bureau. Teva – Advisory Committee/Board Member, Consultant. Topivert – Advisory Committee/Board Member, Consultant. Ventyx – Advisory Committee/Board Member, Consultant. Vividion – Advisory Committee/Board Member, Consultant.
Remo Panaccione, MD, FRCPC1, Talat Bessissow, MDCM, MSc, FRCPC2, Jennifer Glass, PhD3, Theresa Hunter Gibble, PhD, MPH4, Christian Atkinson, BSc, MRes5, Marta Braun, PhD3, Hilary Ellis, BA5, Thomas Dewar, BA5, Vipul Jairath, MBChB, DPhil, FRCPC6. P3633 - Communicating Needs and Features of IBD Experiences (CONFIDE) Survey: Patient and Healthcare Professional Perspectives on Communication Relating to Ulcerative Colitis Symptoms in Canada, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
