Tuesday Poster Session
Category: IBD
P3636 - Risk Factors for Development of Acne for Patients With Inflammatory Bowel Disease Treated With Upadacitinib
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Natalie K. Choi, BA
University of Chicago Medicine, Inflammatory Bowel Disease Center
Los Angeles, CA
Presenting Author(s)
Natalie K. Choi, BA1, David K.. Choi, PharmD1, Nicole M. Garcia, BA1, Scott Friedberg, MD2, Russell D.. Cohen, MD1, David T. Rubin, MD3
1University of Chicago Medicine, Inflammatory Bowel Disease Center, Chicago, IL; 2University of Chicago, Chicago, IL; 3Inflammatory Bowel Disease Center, University of Chicago Medicine, Chicago, IL
Introduction: Upadacitinib (UPA) is a novel, highly selective Janus kinase 1 inhibitor that has received regulatory approval for moderately to severely active ulcerative colitis (UC) and Crohn’s disease (CD). Acne was one of the most frequently reported adverse events (AE) in pivotal trials of UPA for inflammatory bowel disease (IBD) and the most commonly reported AE in our large prospective real-world experience. However, risk factors for acne are not known. Here we present a real-world experience of patient-reported acne as an AE in patients with IBD.
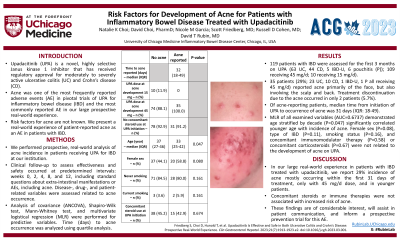
Methods: We performed a prospective, real-world analysis of acne incidence in patients receiving UPA for IBD at our institution. Clinical follow-up to assess effectiveness and safety occurred at predetermined intervals: weeks 0, 2, 4, 8, and 12. This included standard questions about extra-intestinal manifestations or AEs, including acne. Disease-, drug-, and patient-related variables were assessed related to acne occurrence. Analysis of covariance (ANCOVA), Shapiro-Wilk test, Mann-Whitney test, and multivariate logistical regression (MLR) were performed for predictive variables. Time (days) to acne occurrence was analyzed using quartile analysis.
Results: 119 patients with IBD were assessed for the first 3 months on UPA (63 UC, 44 CD, 5 IBD-U, 6 pouchitis (P)); 109 receiving 45 mg/d; 10 receiving 15 mg/d). 35 patients (29%; 23 UC, 10 CD, 1 IBD-U, 1 P all receiving 45 mg/d) reported acne primarily of the face, but also involving the scalp and back. Treatment discontinuation due to the acne occurred in only 2 patients (5.7%). Of acne-reporting patients, the median time from initiation of UPA to occurrence of acne was 31 days (IQR: 18-49). MLR of all examined variables (AUC=0.6737) demonstrated age stratified by decade (P=0.047) significantly correlated younger age with incidence of acne. Female sex (P=0.08), type of IBD (P=0.11), smoking status (P=0.16), and concomitant immunomodulator therapy (P=0.58) or concomitant corticosteroids (P=0.67) were not related to the development of acne on UPA (Table).
Discussion: In our large real-world experience in patients with IBD treated with upadacitinib, we report 29% incidence of acne mostly occurring within the first 31 days of treatment, only with 45 mg/d dose, and in younger patients. Concomitant steroids or immune therapies were not associated with increased risk of acne. These findings are of considerable interest, will assist in patient communication, and inform a prospective prevention trial for this AE.
Disclosures:
Natalie K. Choi, BA1, David K.. Choi, PharmD1, Nicole M. Garcia, BA1, Scott Friedberg, MD2, Russell D.. Cohen, MD1, David T. Rubin, MD3. P3636 - Risk Factors for Development of Acne for Patients With Inflammatory Bowel Disease Treated With Upadacitinib, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Chicago Medicine, Inflammatory Bowel Disease Center, Chicago, IL; 2University of Chicago, Chicago, IL; 3Inflammatory Bowel Disease Center, University of Chicago Medicine, Chicago, IL
Introduction: Upadacitinib (UPA) is a novel, highly selective Janus kinase 1 inhibitor that has received regulatory approval for moderately to severely active ulcerative colitis (UC) and Crohn’s disease (CD). Acne was one of the most frequently reported adverse events (AE) in pivotal trials of UPA for inflammatory bowel disease (IBD) and the most commonly reported AE in our large prospective real-world experience. However, risk factors for acne are not known. Here we present a real-world experience of patient-reported acne as an AE in patients with IBD.
Methods: We performed a prospective, real-world analysis of acne incidence in patients receiving UPA for IBD at our institution. Clinical follow-up to assess effectiveness and safety occurred at predetermined intervals: weeks 0, 2, 4, 8, and 12. This included standard questions about extra-intestinal manifestations or AEs, including acne. Disease-, drug-, and patient-related variables were assessed related to acne occurrence. Analysis of covariance (ANCOVA), Shapiro-Wilk test, Mann-Whitney test, and multivariate logistical regression (MLR) were performed for predictive variables. Time (days) to acne occurrence was analyzed using quartile analysis.
Results: 119 patients with IBD were assessed for the first 3 months on UPA (63 UC, 44 CD, 5 IBD-U, 6 pouchitis (P)); 109 receiving 45 mg/d; 10 receiving 15 mg/d). 35 patients (29%; 23 UC, 10 CD, 1 IBD-U, 1 P all receiving 45 mg/d) reported acne primarily of the face, but also involving the scalp and back. Treatment discontinuation due to the acne occurred in only 2 patients (5.7%). Of acne-reporting patients, the median time from initiation of UPA to occurrence of acne was 31 days (IQR: 18-49). MLR of all examined variables (AUC=0.6737) demonstrated age stratified by decade (P=0.047) significantly correlated younger age with incidence of acne. Female sex (P=0.08), type of IBD (P=0.11), smoking status (P=0.16), and concomitant immunomodulator therapy (P=0.58) or concomitant corticosteroids (P=0.67) were not related to the development of acne on UPA (Table).
Discussion: In our large real-world experience in patients with IBD treated with upadacitinib, we report 29% incidence of acne mostly occurring within the first 31 days of treatment, only with 45 mg/d dose, and in younger patients. Concomitant steroids or immune therapies were not associated with increased risk of acne. These findings are of considerable interest, will assist in patient communication, and inform a prospective prevention trial for this AE.
Disclosures:
Natalie Choi indicated no relevant financial relationships.
David Choi: Abbvie – Consultant. Boehringer Ingelheim – Consultant. Bristol Myers Squibb – Consultant. Janssen Pharmaceuticals – Consultant, Speakers Bureau. Prometheus Laboratory – Consultant.
Nicole Garcia indicated no relevant financial relationships.
Scott Friedberg indicated no relevant financial relationships.
Russell Cohen: AbbVie – Advisor or Review Panel Member, Consultant, Grant/Research Support, Speakers Bureau. Boehringer Ingelheim – Grant/Research Support. Bristol-Meyers Squibb/Celgene – Advisor or Review Panel Member, Consultant, Grant/Research Support. Crohn's and Colitis Foundation of America – Grant/Research Support. Eli Lilly – Advisor or Review Panel Member, Consultant. Genentech – Advisor or Review Panel Member, Consultant, Grant/Research Support. Gilead Sciences – Advisor or Review Panel Member, Consultant, Grant/Research Support. Hoffman La-Roche – Advisor or Review Panel Member, Consultant. Hollister – Grant/Research Support. Janssen – Advisor or Review Panel Member, Consultant. Medimmune – Grant/Research Support. Mesoblast, Ltd. – Grant/Research Support. Osiris Therapeutics – Grant/Research Support. Pfizer – Advisor or Review Panel Member, Consultant, Grant/Research Support. Receptos – Grant/Research Support. RedHill BioPharma – Grant/Research Support. Sanofi-Aventis – Grant/Research Support. Schwarz Pharma – Grant/Research Support. Seres Therapeutics – Grant/Research Support. Takeda – Advisor or Review Panel Member, Consultant, Grant/Research Support, Speakers Bureau.
David Rubin: AbbVie – Consultant, personal fees. AltruBio – Consultant, personal fees. Aslan Pharmaceuticals – Consultant. Athos Therapeutics – Consultant. Bellatrix Pharmaceuticals – Consultant. Boehringer Ingelheim – Consultant, personal fees. Bristol Myers Squibb – Consultant. Celgene Chronicles – Consultant. ClostraBio – Consultant. Connect BioPharma – Consultant. Corp/Syneos – Consultant. Eco R1 – Consultant. GastroIntestinal Research Foundation – Grant/Research Support. Genentech/Roche – Consultant. Gilead Sciences – Consultant, personal fees. Helmsley Charitable Trust – Grant/Research Support. Iterative Health – Consultant. Janssen Pharmaceuticals – Consultant, personal fees. Kaleido Biosciences – Consultant. Lilly – Consultant. Pfizer – Consultant, personal fees. Prometheus Biosciences – Consultant. Reistone Biopharma – Consultant, personal fees. Seres Therapeutics – Consultant. Takeda – Consultant, Grant/Research Support, Personal fees. Target RWE – Consultant. Trellus Health – Consultant.
Natalie K. Choi, BA1, David K.. Choi, PharmD1, Nicole M. Garcia, BA1, Scott Friedberg, MD2, Russell D.. Cohen, MD1, David T. Rubin, MD3. P3636 - Risk Factors for Development of Acne for Patients With Inflammatory Bowel Disease Treated With Upadacitinib, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

