Tuesday Poster Session
Category: IBD
P3645 - Clinical Decision Making in Mimickers of IBD: Practice Management From IBD Live
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Hannah W. Fiske, MD
Brown University/Rhode Island Hospital
Providence, RI
Presenting Author(s)
Hannah W. Fiske, MD1, Christopher Ward, MD2, Samir A. Shah, MD, FACG3, David Binion, MD, FACG4, Steven Wexner, MD, PhD5, Francis A. Farraye, MD, MSc, MACG6, Alka Goyal, MBBS, MD7, Jeffrey M. Dueker, MD, MPH4, John S. Hanson, MD8, Raymond K.. Cross, MD, MS, FACG9, Corey A. Siegel, MD, MS10, Badr Al-Bawardy, MD11, Edward Barnes, MD, MPH, FACG12, Myron Brand, MD, FACG13, Joanna MP. Melia, MD14, Kofi Clarke, MD15, Philip M. Ginsburg, MD, FACG16, Hans Herfarth, MD, PhD12, Erin Forster, MD, MPH17, Mike Engels, MD18, Taha Qazi, MD19, Matthew Bohm, DO20, Ben Cohen, MD, MAS21, Aamir Dam, MD22, Sean Fine, MD, MS23, Jill Gaidos, MD, FACG24, Stefan Holubar, MD21, Tracy L. Hull, MD25, Colleen R.. Kelly, MD26, L. Campbell Levy, MD27, Jessica Philpott, MD, PhD28, Miguel Regueiro, MD29
1Brown University/Rhode Island Hospital, Providence, RI; 2Lahey Clinic, Lahey, MA; 3Gastroenterology Associates, Inc., Providence, RI; 4UPMC, Pittsburgh, PA; 5Cleveland Clinic Florida, Weston, FL; 6Mayo Clinic, Jacksonville, FL; 7Stanford University, Palo Alto, CA; 8Atrium Health, Charlotte, NC; 9University of Maryland School of Medicine, Baltimore, MD; 10Dartmouth-Hitchcock Inflammatory Bowel Disease Center, Dartmouth-Hitchcock Medical Center, Lebanon, NH; 11King Faisal Specialist Hospital and Research Center, Riyadh, Ar Riyad, Saudi Arabia; 12University of North Carolina at Chapel Hill, Chapel Hill, NC; 13Yale University, Guilford, CT; 14Johns Hopkins University School of Medicine, Baltimore, MD; 15Penn State Health, Hershey, PA; 16Yale University School of Medicine, Hamden, CT; 17Medical University of South Carolina, Charleston, SC; 18Lehigh Valley Hospital, Allentown, PA; 19Digestive Disease and Surgery Institute, Cleveland Clinic, Cleveland, OH; 20Indiana University Hospital, Indianapolis, IN; 21Cleveland Clinic, Cleveland, OH; 22Moffitt Cancer Center, Tampa, FL; 23Warren Alpert Medical School of Brown University, Providence, RI; 24Yale University, New Haven, CT; 25Cleveland Clinic, Chagrin Falls, OH; 26Alpert School of Medicine of Brown University, Providence, RI; 27Dartmouth Hitchcock Medical Center, Lebanon, NH; 28Cleveland Clinic Foundation, Cleveland, OH; 29Cleveland Clinic Lerner College of Medicine, Case Western Reserve University, Cleveland, OH
Introduction: Since 2009, a group of inflammatory bowel disease (IBD) specialists have been utilizing “IBD Live,” a weekly live video conference with a global audience of 150-200 participants, to discuss the multidisciplinary management of their most challenging cases. While most cases presented were confirmed as IBD, a substantial number were mimics for which IBD was not the ultimate diagnosis. We have prospectively categorized all IBD Live cases and identified “IBD mimics” with consequent clinical management implications.
Methods: Cases have been recorded and archived since May 2018. 371 total cases from May 2018 through February 2023 were reviewed spanning 186 hours. IBD mimics were defined as those cases with features of IBD that ultimately resulted in a non-IBD diagnosis. IBD mimics were analysed and categorized by original suspected diagnosis, diagnostic workup, and the evaluation that led to the correct diagnosis.
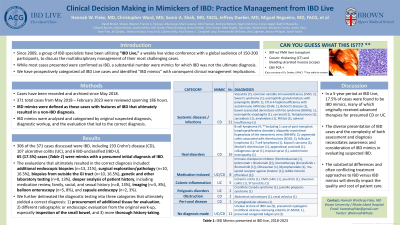
Results: 306 of the 371 cases discussed were IBD including 193 Crohn’s disease (CD), 107 ulcerative colitis (UC) and 6 IBD-unclassified (IBD-U). 65 (17.5%) cases (Table 1) were mimics with a presumed initial diagnosis of IBD.
The evaluations that ultimately resulted in the correct diagnosis included: additional endoscopic biopsies (n=13, 21%), surgical exploration/pathology (n=10, 16.5%), biopsies from outside the GI tract (n=10, 16.5%), genetic and other laboratory testing (n=8, 13%), deeper analysis of patient history, including medication review, family, social, and sexual history (n=8, 13%), imaging (n=5, 8%), balloon enteroscopy (n=5, 8%), and capsule endoscopy (n=2, 3%).
We further delineated the diagnostic testing into three categories that ultimately yielded a correct diagnosis: 1) procurement of additional tissue for evaluation, 2) different radiographic or endoscopic evaluation from the original work-up, especially inspection of the small bowel, and 3) more thorough history-taking.
Discussion: In a 5-year period at IBD Live, 17.5% of cases were found to be IBD mimics, many of which originally received advanced therapies for presumed CD or UC. The diverse presentation of IBD cases and the complexity of both assessment and diagnosis necessitates significant consideration of IBD mimics at all times. The substantial differences and often conflicting treatment approaches to IBD versus IBD mimics will directly impact the quality and cost of patient care.
Disclosures:
Hannah W. Fiske, MD1, Christopher Ward, MD2, Samir A. Shah, MD, FACG3, David Binion, MD, FACG4, Steven Wexner, MD, PhD5, Francis A. Farraye, MD, MSc, MACG6, Alka Goyal, MBBS, MD7, Jeffrey M. Dueker, MD, MPH4, John S. Hanson, MD8, Raymond K.. Cross, MD, MS, FACG9, Corey A. Siegel, MD, MS10, Badr Al-Bawardy, MD11, Edward Barnes, MD, MPH, FACG12, Myron Brand, MD, FACG13, Joanna MP. Melia, MD14, Kofi Clarke, MD15, Philip M. Ginsburg, MD, FACG16, Hans Herfarth, MD, PhD12, Erin Forster, MD, MPH17, Mike Engels, MD18, Taha Qazi, MD19, Matthew Bohm, DO20, Ben Cohen, MD, MAS21, Aamir Dam, MD22, Sean Fine, MD, MS23, Jill Gaidos, MD, FACG24, Stefan Holubar, MD21, Tracy L. Hull, MD25, Colleen R.. Kelly, MD26, L. Campbell Levy, MD27, Jessica Philpott, MD, PhD28, Miguel Regueiro, MD29. P3645 - Clinical Decision Making in Mimickers of IBD: Practice Management From IBD Live, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Brown University/Rhode Island Hospital, Providence, RI; 2Lahey Clinic, Lahey, MA; 3Gastroenterology Associates, Inc., Providence, RI; 4UPMC, Pittsburgh, PA; 5Cleveland Clinic Florida, Weston, FL; 6Mayo Clinic, Jacksonville, FL; 7Stanford University, Palo Alto, CA; 8Atrium Health, Charlotte, NC; 9University of Maryland School of Medicine, Baltimore, MD; 10Dartmouth-Hitchcock Inflammatory Bowel Disease Center, Dartmouth-Hitchcock Medical Center, Lebanon, NH; 11King Faisal Specialist Hospital and Research Center, Riyadh, Ar Riyad, Saudi Arabia; 12University of North Carolina at Chapel Hill, Chapel Hill, NC; 13Yale University, Guilford, CT; 14Johns Hopkins University School of Medicine, Baltimore, MD; 15Penn State Health, Hershey, PA; 16Yale University School of Medicine, Hamden, CT; 17Medical University of South Carolina, Charleston, SC; 18Lehigh Valley Hospital, Allentown, PA; 19Digestive Disease and Surgery Institute, Cleveland Clinic, Cleveland, OH; 20Indiana University Hospital, Indianapolis, IN; 21Cleveland Clinic, Cleveland, OH; 22Moffitt Cancer Center, Tampa, FL; 23Warren Alpert Medical School of Brown University, Providence, RI; 24Yale University, New Haven, CT; 25Cleveland Clinic, Chagrin Falls, OH; 26Alpert School of Medicine of Brown University, Providence, RI; 27Dartmouth Hitchcock Medical Center, Lebanon, NH; 28Cleveland Clinic Foundation, Cleveland, OH; 29Cleveland Clinic Lerner College of Medicine, Case Western Reserve University, Cleveland, OH
Introduction: Since 2009, a group of inflammatory bowel disease (IBD) specialists have been utilizing “IBD Live,” a weekly live video conference with a global audience of 150-200 participants, to discuss the multidisciplinary management of their most challenging cases. While most cases presented were confirmed as IBD, a substantial number were mimics for which IBD was not the ultimate diagnosis. We have prospectively categorized all IBD Live cases and identified “IBD mimics” with consequent clinical management implications.
Methods: Cases have been recorded and archived since May 2018. 371 total cases from May 2018 through February 2023 were reviewed spanning 186 hours. IBD mimics were defined as those cases with features of IBD that ultimately resulted in a non-IBD diagnosis. IBD mimics were analysed and categorized by original suspected diagnosis, diagnostic workup, and the evaluation that led to the correct diagnosis.
Results: 306 of the 371 cases discussed were IBD including 193 Crohn’s disease (CD), 107 ulcerative colitis (UC) and 6 IBD-unclassified (IBD-U). 65 (17.5%) cases (Table 1) were mimics with a presumed initial diagnosis of IBD.
The evaluations that ultimately resulted in the correct diagnosis included: additional endoscopic biopsies (n=13, 21%), surgical exploration/pathology (n=10, 16.5%), biopsies from outside the GI tract (n=10, 16.5%), genetic and other laboratory testing (n=8, 13%), deeper analysis of patient history, including medication review, family, social, and sexual history (n=8, 13%), imaging (n=5, 8%), balloon enteroscopy (n=5, 8%), and capsule endoscopy (n=2, 3%).
We further delineated the diagnostic testing into three categories that ultimately yielded a correct diagnosis: 1) procurement of additional tissue for evaluation, 2) different radiographic or endoscopic evaluation from the original work-up, especially inspection of the small bowel, and 3) more thorough history-taking.
Discussion: In a 5-year period at IBD Live, 17.5% of cases were found to be IBD mimics, many of which originally received advanced therapies for presumed CD or UC. The diverse presentation of IBD cases and the complexity of both assessment and diagnosis necessitates significant consideration of IBD mimics at all times. The substantial differences and often conflicting treatment approaches to IBD versus IBD mimics will directly impact the quality and cost of patient care.
Disclosures:
Hannah Fiske indicated no relevant financial relationships.
Christopher Ward indicated no relevant financial relationships.
Samir Shah indicated no relevant financial relationships.
David Binion: Abbvie – Grant/Research Support. Merck – Grant/Research Support. Sanofi – Consultant. Takeda – Grant/Research Support.
Steven Wexner: ARC/Corvus – Consultant. Astellas – Consultant. Baxter – Consultant. Becton Dickinson – Consultant. GI Supply – Consultant. ICON Language Services – Consultant. Intuitive Surgical – Consultant. Intuitive Surgical – Royalties. Karl Storz Endoscopy – Royalties. Leading BioSciences – Consultant. Medtronic – Consultant. Olympus – Consultant. Stryker – Consultant. Takeda – Consultant.
Francis Farraye: AbbVie – Advisory Committee/Board Member. Avalo Therapeutics – Advisory Committee/Board Member. BMS – Advisory Committee/Board Member. Braintree Labs – Advisory Committee/Board Member. Fresenius Kabi – Advisory Committee/Board Member. GI Reviewers – Independent Contractor. GSK – Advisory Committee/Board Member. IBD Educational Group – Independent Contractor. Iterative Health – Advisory Committee/Board Member. Janssen – Advisory Committee/Board Member. Pfizer – Advisory Committee/Board Member. Pharmacosmos – Advisory Committee/Board Member. Sandoz Immunology – Advisory Committee/Board Member. Sebela – Advisory Committee/Board Member. Viatris – Advisory Committee/Board Member.
Alka Goyal indicated no relevant financial relationships.
Jeffrey Dueker indicated no relevant financial relationships.
John Hanson indicated no relevant financial relationships.
Raymond Cross: AbbVie – Consultant. Bristol Myers Squibb – Consultant. Janssen – Consultant. LabCorp – Consultant. Pfizer – Consultant. Samsung Bioepis – Consultant. Takeda – Consultant.
Corey Siegel: Abbvie – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. BMS – Advisory Committee/Board Member, Consultant. Eli Lilly – Advisory Committee/Board Member, Consultant. Fresnius – Advisory Committee/Board Member, Consultant. Janssen – Advisory Committee/Board Member, Consultant, Grant/Research Support, Consultant/advisory board, speaker for CME activities. Napo Pharmaceuticals – Advisory Committee/Board Member, Consultant. Pfizer – Advisory Committee/Board Member, Consultant, Grant/Research Support, speaker for CME activities. Prometheus Biosciences – Advisory Committee/Board Member, Consultant. Takeda – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau.
Badr Al-Bawardy: AbbVie – Speakers Bureau. Bristol Myers Squibb – Advisor or Review Panel Member, Speakers Bureau. Pfizer – Advisor or Review Panel Member. Takeda – Speakers Bureau.
Edward Barnes: AbbVie, Inc. – Consultant. Bristol-Meyers Squibb – Consultant. Eli Lilly – Consultant. Target RWE – Consultant.
Myron Brand indicated no relevant financial relationships.
Joanna Melia: Janssen – Grant/Research Support. Pfizer – Grant/Research Support.
Kofi Clarke: ABBVie – Consultant, Speakers Bureau. Janssen – Advisory Committee/Board Member, Speakers Bureau. Takeda – Speakers Bureau.
Philip Ginsburg: Abbvie Immunology – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. Amgen – Grant/Research Support. Bristol-Myers Squibb – Grant/Research Support, Speakers Bureau. Eli Lilly and Company – Grant/Research Support. Fresenius Kabi Immunology – Advisory Committee/Board Member. Hoffmann LaRoche – Grant/Research Support. Janssen Pharmaceuticals – Grant/Research Support, Speakers Bureau. Pfizer, Inc – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. ProciseDx Inc – Grant/Research Support. Prometheus Biosciences – Grant/Research Support. Takeda Pharmeceuticals – Grant/Research Support, Speakers Bureau.
Hans Herfarth: BMS – Consultant. EXE-GI – Consultant. Fresenius Kabi – Consultant. Galapagos – Consultant. Gilead – Consultant. Janssen – Consultant. NovoNordisk – Grant/Research Support. Pfizer – Grant/Research Support. Ventyx – Consultant.
Erin Forster: Abbvie – Speakers Bureau. BMS – Speakers Bureau. Takeda – Speakers Bureau.
Mike Engels: Abbvie – Speakers Bureau. Bristol Meyers Squibb – Advisory Committee/Board Member. Pfizer – Speakers Bureau.
Taha Qazi: Abbvie – Advisor or Review Panel Member, Speakers Bureau. BMS – Advisor or Review Panel Member, Speakers Bureau. Itierative Scope – Advisor or Review Panel Member. Janssen – Speakers Bureau.
Matthew Bohm indicated no relevant financial relationships.
Ben Cohen indicated no relevant financial relationships.
Aamir Dam indicated no relevant financial relationships.
Sean Fine: AbbVie – Advisory Committee/Board Member, Consultant. Bristol Myers Squibb – Advisory Committee/Board Member, Consultant.
Jill Gaidos: Abbvie – Advisor or Review Panel Member, Grant/Research Support. Bristol Myers Squibb – Grant/Research Support. Pfizer – Consultant, Grant/Research Support.
Stefan Holubar: Guidepoint – Consultant. Takeda – Consultant.
Tracy Hull indicated no relevant financial relationships.
Colleen Kelly: Sebela Pharmaceuticals – Consultant.
L. Campbell Levy indicated no relevant financial relationships.
Jessica Philpott: Abbvie – Speakers Bureau.
Miguel Regueiro: AbbVie – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Alfasigma – Advisory Committee/Board Member, Consultant. Allergan – Advisory Committee/Board Member, Consultant. Amgen – Advisory Committee/Board Member, Consultant. Bristol Myers Squibb – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Celgene – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Eli Lilly – Advisory Committee/Board Member, Consultant. Genentech – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Gilead Sciences – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Janssen – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Miraca Labs – Advisory Committee/Board Member, Consultant. Pfizer Inc – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Prometheus – Advisory Committee/Board Member, Consultant. Salix – Advisory Committee/Board Member, Consultant. Seres – Advisory Committee/Board Member, Consultant. Takeda – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Target RWE – Advisory Committee/Board Member, Consultant. UCB – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Wolters Kluwer Health – Royalties.
Hannah W. Fiske, MD1, Christopher Ward, MD2, Samir A. Shah, MD, FACG3, David Binion, MD, FACG4, Steven Wexner, MD, PhD5, Francis A. Farraye, MD, MSc, MACG6, Alka Goyal, MBBS, MD7, Jeffrey M. Dueker, MD, MPH4, John S. Hanson, MD8, Raymond K.. Cross, MD, MS, FACG9, Corey A. Siegel, MD, MS10, Badr Al-Bawardy, MD11, Edward Barnes, MD, MPH, FACG12, Myron Brand, MD, FACG13, Joanna MP. Melia, MD14, Kofi Clarke, MD15, Philip M. Ginsburg, MD, FACG16, Hans Herfarth, MD, PhD12, Erin Forster, MD, MPH17, Mike Engels, MD18, Taha Qazi, MD19, Matthew Bohm, DO20, Ben Cohen, MD, MAS21, Aamir Dam, MD22, Sean Fine, MD, MS23, Jill Gaidos, MD, FACG24, Stefan Holubar, MD21, Tracy L. Hull, MD25, Colleen R.. Kelly, MD26, L. Campbell Levy, MD27, Jessica Philpott, MD, PhD28, Miguel Regueiro, MD29. P3645 - Clinical Decision Making in Mimickers of IBD: Practice Management From IBD Live, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
