Monday Poster Session
Category: Biliary/Pancreas
P1430 - Lack of Standardized Assessment of Malnutrition in Chronic Pancreatitis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Sukrit Jain, MD
Duke University
Durham, NC
Presenting Author(s)
Sukrit Jain, MD1, Elizabeth Lilley, MD, MPH1, Darshan Kothari, MD2
1Duke University, Durham, NC; 2Duke University School of Medicine, Durham VA Medical Center, Durham, NC
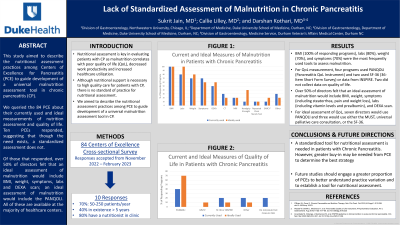
Introduction: Nutritional assessment is key in evaluating patients with chronic pancreatitis (CP) as malnutrition correlates with poor quality of life (QoL), work productivity and increased healthcare utilization. Although experts agree that nutritional support is necessary to high quality care for patients with CP, there is no standard of practice for nutritional assessment. In this study, we aimed to describe the nutritional assessment practices among Centers of Excellence for CP (PCE) to guide development of a universal malnutrition assessment tool in CP.
Methods: We performed a descriptive, cross-sectional study by querying all the US PCE, as designated by the National Pancreas Foundation, on their nutritional assessment practices. Responses were accepted from November 2022 – February 2023. We received responses from 10 of 80 PCE. 70% of PCE saw between 50 - 250 patients per year and 40% had been in existence for greater than 5 years.
Results: The most frequently used tools for assessment of malnutrition included BMI (100% of responding programs), labs (80%), weight (73%), and symptoms (73%). Centers used steatorrhea, weight loss and abdominal pain as hallmark symptoms of malnutrition and often measured fat-soluble vitamins, vitamin B12, and prealbumin for assessment of malnutrition. More than half of directors felt that an ideal assessment of malnutrition would include BMI, weight, symptoms (including presence of steatorrhea, pain and weight loss), labs (including vitamin levels and prealbumin), and DEXA scan. For QoL measurement, four programs used PANQOLI (Pancreatitis QoL Instrument) and three used SF-36 (36-Item Short Form Survey) or data from INSPIRE. Two programs did not measure QoL. In describing ideal practices, seven directors would use PANQOLI and three would use either the MUST, universal palliative care consultation, or the SF-36. Though all centers are required to have access to a registered dietician, only 8 of 10 programs had a dietician in their clinic.
Discussion: In our cross-sectional study, we received about 13% of PCE responses, which suggests that though the need exists, a standardized assessment does not. Our analysis demonstrated that the majority of PCE directors surveyed felt that an ideal assessment of malnutrition in patients with CP would include BMI, weight, symptoms, vitamin levels, prealbumin, and DEXA scan with the PANQOLI being an ideal measure of QoL, all of which are available at the majority of healthcare centers.
Disclosures:
Sukrit Jain, MD1, Elizabeth Lilley, MD, MPH1, Darshan Kothari, MD2. P1430 - Lack of Standardized Assessment of Malnutrition in Chronic Pancreatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Duke University, Durham, NC; 2Duke University School of Medicine, Durham VA Medical Center, Durham, NC
Introduction: Nutritional assessment is key in evaluating patients with chronic pancreatitis (CP) as malnutrition correlates with poor quality of life (QoL), work productivity and increased healthcare utilization. Although experts agree that nutritional support is necessary to high quality care for patients with CP, there is no standard of practice for nutritional assessment. In this study, we aimed to describe the nutritional assessment practices among Centers of Excellence for CP (PCE) to guide development of a universal malnutrition assessment tool in CP.
Methods: We performed a descriptive, cross-sectional study by querying all the US PCE, as designated by the National Pancreas Foundation, on their nutritional assessment practices. Responses were accepted from November 2022 – February 2023. We received responses from 10 of 80 PCE. 70% of PCE saw between 50 - 250 patients per year and 40% had been in existence for greater than 5 years.
Results: The most frequently used tools for assessment of malnutrition included BMI (100% of responding programs), labs (80%), weight (73%), and symptoms (73%). Centers used steatorrhea, weight loss and abdominal pain as hallmark symptoms of malnutrition and often measured fat-soluble vitamins, vitamin B12, and prealbumin for assessment of malnutrition. More than half of directors felt that an ideal assessment of malnutrition would include BMI, weight, symptoms (including presence of steatorrhea, pain and weight loss), labs (including vitamin levels and prealbumin), and DEXA scan. For QoL measurement, four programs used PANQOLI (Pancreatitis QoL Instrument) and three used SF-36 (36-Item Short Form Survey) or data from INSPIRE. Two programs did not measure QoL. In describing ideal practices, seven directors would use PANQOLI and three would use either the MUST, universal palliative care consultation, or the SF-36. Though all centers are required to have access to a registered dietician, only 8 of 10 programs had a dietician in their clinic.
Discussion: In our cross-sectional study, we received about 13% of PCE responses, which suggests that though the need exists, a standardized assessment does not. Our analysis demonstrated that the majority of PCE directors surveyed felt that an ideal assessment of malnutrition in patients with CP would include BMI, weight, symptoms, vitamin levels, prealbumin, and DEXA scan with the PANQOLI being an ideal measure of QoL, all of which are available at the majority of healthcare centers.
Disclosures:
Sukrit Jain indicated no relevant financial relationships.
Elizabeth Lilley indicated no relevant financial relationships.
Darshan Kothari indicated no relevant financial relationships.
Sukrit Jain, MD1, Elizabeth Lilley, MD, MPH1, Darshan Kothari, MD2. P1430 - Lack of Standardized Assessment of Malnutrition in Chronic Pancreatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
