Monday Poster Session
Category: Biliary/Pancreas
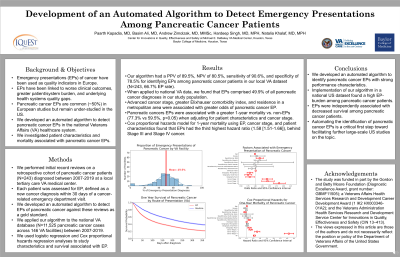
P1433 - Development of an Automated Algorithm to Detect Emergency Presentations Among Pancreatic Cancer Patients
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Paarth Kapadia, MD
University of Pittsburgh Medical Center
Pittsburgh, PA
Presenting Author(s)
Paarth Kapadia, MD1, Basim Ali, MD2, Andrew Zimolzak, MD3, Hardeep Singh, MD, MPH3, Natalia Khalaf, MD, MPH3
1University of Pittsburgh Medical Center, Pittsburgh, PA; 2Baylor College of Medicine, Houston, TX; 3Baylor College of Medicine / Michael E. DeBakey Veterans Affairs Medical Center, Houston, TX
Introduction: Cancer diagnosis via emergency presentation (EP) is associated with inferior patient outcomes. Pancreatic cancer has among the highest rates of EPs in European studies; however, such EPs remain underexplored in the U.S. In this study, we developed an automated algorithm to detect pancreatic cancer EPs in the national Veterans Affairs (VA) healthcare system and investigated patient characteristics and survival associated with EPs.
Methods:
Results:
Discussion:
Disclosures:
Paarth Kapadia, MD1, Basim Ali, MD2, Andrew Zimolzak, MD3, Hardeep Singh, MD, MPH3, Natalia Khalaf, MD, MPH3. P1433 - Development of an Automated Algorithm to Detect Emergency Presentations Among Pancreatic Cancer Patients, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Pittsburgh Medical Center, Pittsburgh, PA; 2Baylor College of Medicine, Houston, TX; 3Baylor College of Medicine / Michael E. DeBakey Veterans Affairs Medical Center, Houston, TX
Introduction: Cancer diagnosis via emergency presentation (EP) is associated with inferior patient outcomes. Pancreatic cancer has among the highest rates of EPs in European studies; however, such EPs remain underexplored in the U.S. In this study, we developed an automated algorithm to detect pancreatic cancer EPs in the national Veterans Affairs (VA) healthcare system and investigated patient characteristics and survival associated with EPs.
Methods:
We performed record reviews on a retrospective cohort of pancreatic cancer patients (N=243) diagnosed between 2007-2019 at a local tertiary care VA medical center. We classified each patient by EP status (yes/no). An EP was defined as a new cancer diagnosis within 30 days of a cancer-related emergency department visit. Using these reviews as a gold standard, we developed, tested, and iteratively refined an automated algorithm to detect pancreatic cancer EPs and applied this algorithm to the national VA database (N=11,525 pancreatic cancer cases across 146 VA facilities) between 2007-2019. We used logistic regression analysis to study sociodemographic and clinical characteristics associated with EPs and Cox proportional hazards regression models to study survival by EP status.
Results:
The algorithm had a positive predictive value of 89.5%, negative predictive value of 80.5%, sensitivity of 90.6%, and specificity of 78.5% for identifying EPs among pancreatic cancer patients in the local VA dataset (N=243, 66.7% EP rate). In national VA data, the algorithm identified EPs in 5,751 out of 11,525 (49.9%) newly diagnosed pancreatic cancer cases between 2007-2019. In multivariable logistic regression, advanced stage disease was associated with EPs (Table 1). One-year mortality for EPs was 77.3% compared to 59.4% for non-EPs with a hazard ratio of 1.58 (95% confidence interval 1.51-1.66) after adjusting for cancer stage, age, race, sex, and rurality.
Discussion:
We developed an automated algorithm to identify pancreatic cancer EPs in a national U.S. healthcare system with strong performance characteristics. We found that EPs of pancreatic cancer were common, particularly in advanced stage diagnoses, and independently associated with decreased survival. This is a critical first step toward facilitating further large-scale U.S. EP studies by automating the laborious manual review process for identifying EPs. Enhanced understanding of factors contributing to EPs can help identify care gaps and guide interventions to prevent EPs and reduce related harms.
Disclosures:
Paarth Kapadia indicated no relevant financial relationships.
Basim Ali indicated no relevant financial relationships.
Andrew Zimolzak indicated no relevant financial relationships.
Hardeep Singh indicated no relevant financial relationships.
Natalia Khalaf indicated no relevant financial relationships.
Paarth Kapadia, MD1, Basim Ali, MD2, Andrew Zimolzak, MD3, Hardeep Singh, MD, MPH3, Natalia Khalaf, MD, MPH3. P1433 - Development of an Automated Algorithm to Detect Emergency Presentations Among Pancreatic Cancer Patients, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
