Monday Poster Session
Category: Biliary/Pancreas
P1441 - Transfer Utilization and Outcomes of Patients with Acute Pancreatitis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Thuy-Duyen Nguyen, MD
Oregon Health & Science University
Portland, OR
Presenting Author(s)
Thuy-Duyen Nguyen, MD, Jennifer Rodriguez, MD, Melissa Chai, MD, Steven Koprowski, MD, Saad Jazrawi, MD, Gennadiy Bakis, MD, Kaveh Sharzehi, MD, MS, Emily Jonica, MD, Gregory Cote, MD, MS, Jessica X. Yu, MD, MS
Oregon Health & Science University, Portland, OR
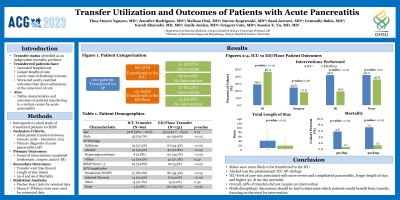
Introduction: Acute pancreatitis (AP) is the most common GI diagnosis requiring inpatient admission with rising global incidence. Treatment is complex, often requiring the transfer of patients to centers with access to subspecialty GI care. Utilization of such transfers is resource-intensive and poorly understood. We sought to define characteristics and outcomes of patients transferring to a tertiary referral center with AP.
Methods: We conducted a retrospective study of patients transferred to a single tertiary referral center. We identified all adult patients transferred from January 2018–December 2021 for AP using ICD 9 (577.0) and 10 codes (K85.x). Demographics, time awaiting transfer, length of stay, forms of interventions completed (endoscopic, surgery, and IR), and mortality were obtained. Fisher exact and Mann-U-Whitney tests were used for nominal and numerical statistical analysis, respectively.
Results: 220 patients were transferred for AP. Median age was 53 years (IQR 42-62). 75 (34%) were female. The most common AP etiologies were gallstone disease (n=86, 39%) and alcohol use (n=73, 33%). In our cohort, 69 (31%) were transferred to the ICU. 54 (24%) developed pseudocysts or walled-off pancreatic necrosis (WOPN), 17 (8%) infected necrosis, and 30 (14%) had other complications (e.g. ARDS, thrombosis, etc.). Of the 220 patients, 60 (27%) had an IR procedure, 44 (20%) underwent surgery, and 90 (41%) had a pancreaticobiliary endoscopy. Median length of stay for all patients was 10 days (IQR 5-23). The 30-day mortality rate was 2.3% (n=5), and 90-day mortality rate was 3.2% (n=7). Patients transferred to the ICU had a higher 30-day mortality (p = 0.035) and higher 90-day mortality (p = 0.005), as well as increased likelihood of requiring either endoscopic intervention (p = 0.018), surgical intervention (p = 0.27), and/or intervention with interventional radiology (p = 0.002) (Table 1).
Discussion: Pancreatitis imposes a significant burden on our medical system. Our study shows that patients with acute pancreatitis who require transfer to a tertiary medical center have prolonged hospital stays associated with ICU-level care, complex medical and surgical interventions, and increased mortality and readmission rates. Efforts to intervene for these high-risk patients are needed.
Disclosures:
Thuy-Duyen Nguyen, MD, Jennifer Rodriguez, MD, Melissa Chai, MD, Steven Koprowski, MD, Saad Jazrawi, MD, Gennadiy Bakis, MD, Kaveh Sharzehi, MD, MS, Emily Jonica, MD, Gregory Cote, MD, MS, Jessica X. Yu, MD, MS. P1441 - Transfer Utilization and Outcomes of Patients with Acute Pancreatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Oregon Health & Science University, Portland, OR
Introduction: Acute pancreatitis (AP) is the most common GI diagnosis requiring inpatient admission with rising global incidence. Treatment is complex, often requiring the transfer of patients to centers with access to subspecialty GI care. Utilization of such transfers is resource-intensive and poorly understood. We sought to define characteristics and outcomes of patients transferring to a tertiary referral center with AP.
Methods: We conducted a retrospective study of patients transferred to a single tertiary referral center. We identified all adult patients transferred from January 2018–December 2021 for AP using ICD 9 (577.0) and 10 codes (K85.x). Demographics, time awaiting transfer, length of stay, forms of interventions completed (endoscopic, surgery, and IR), and mortality were obtained. Fisher exact and Mann-U-Whitney tests were used for nominal and numerical statistical analysis, respectively.
Results: 220 patients were transferred for AP. Median age was 53 years (IQR 42-62). 75 (34%) were female. The most common AP etiologies were gallstone disease (n=86, 39%) and alcohol use (n=73, 33%). In our cohort, 69 (31%) were transferred to the ICU. 54 (24%) developed pseudocysts or walled-off pancreatic necrosis (WOPN), 17 (8%) infected necrosis, and 30 (14%) had other complications (e.g. ARDS, thrombosis, etc.). Of the 220 patients, 60 (27%) had an IR procedure, 44 (20%) underwent surgery, and 90 (41%) had a pancreaticobiliary endoscopy. Median length of stay for all patients was 10 days (IQR 5-23). The 30-day mortality rate was 2.3% (n=5), and 90-day mortality rate was 3.2% (n=7). Patients transferred to the ICU had a higher 30-day mortality (p = 0.035) and higher 90-day mortality (p = 0.005), as well as increased likelihood of requiring either endoscopic intervention (p = 0.018), surgical intervention (p = 0.27), and/or intervention with interventional radiology (p = 0.002) (Table 1).
Discussion: Pancreatitis imposes a significant burden on our medical system. Our study shows that patients with acute pancreatitis who require transfer to a tertiary medical center have prolonged hospital stays associated with ICU-level care, complex medical and surgical interventions, and increased mortality and readmission rates. Efforts to intervene for these high-risk patients are needed.
Disclosures:
Thuy-Duyen Nguyen indicated no relevant financial relationships.
Jennifer Rodriguez indicated no relevant financial relationships.
Melissa Chai indicated no relevant financial relationships.
Steven Koprowski indicated no relevant financial relationships.
Saad Jazrawi indicated no relevant financial relationships.
Gennadiy Bakis indicated no relevant financial relationships.
Kaveh Sharzehi indicated no relevant financial relationships.
Emily Jonica indicated no relevant financial relationships.
Gregory Cote: Interpace Diagnostics – Consultant. Olympus Corporation – Consultant.
Jessica Yu indicated no relevant financial relationships.
Thuy-Duyen Nguyen, MD, Jennifer Rodriguez, MD, Melissa Chai, MD, Steven Koprowski, MD, Saad Jazrawi, MD, Gennadiy Bakis, MD, Kaveh Sharzehi, MD, MS, Emily Jonica, MD, Gregory Cote, MD, MS, Jessica X. Yu, MD, MS. P1441 - Transfer Utilization and Outcomes of Patients with Acute Pancreatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
