Monday Poster Session
Category: Biliary/Pancreas
P1445 - Aggressive versus Moderate Fluid Replacement for Acute Pancreatitis: An Updated Systematic Review and Meta-Analysis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Sophia Dar, MD
Northshore-Long Island Jewish Medical Center
Springfield , IL
Presenting Author(s)
Muhammad Ehsan, MBBS1, Aamna Badar Ahmad, MBBS1, Muhammad Ayyan, MBBS1, Afra Zahid, MBBS1, Haseeba Javed, MBBS1, Hafiz Sheheryar Aamir, MBBS1, Biah Mustafa, MBBS1, Huzaifa Ahmad Cheema, MBBS1, Abia Shahid, MBBS1, Muhammad Abdullah Ilyas, MBBS1, Sophia Haroon Dar, MD2, Rehmat Ullah Awan, MD3
1King Edward Medical University, Lahore, Punjab, Pakistan; 2Northshore-Long Island Jewish Medical Center, New York, NY; 3Ochsner Rush Medical Center, Meridian, MS
Introduction: Fluid replacement is the primary modality of treatment for acute pancreatitis. Since the results regarding aggressive versus moderate fluid replenishment for acute pancreatitis are inconsistent, we sought to compare patient outcomes between the two fluid resuscitation groups to determine the superior resuscitation protocol in our meta-analysis.
Methods: We searched MEDLINE (PubMed), Embase, International Clinical Trials Registry Platform (ICTRP), Cochrane Central Register of Controlled Trials, and Google Scholar for all available randomized controlled trials (RCTs) assessing the outcomes for patients treated using different protocols of fluids resuscitation with the aggressive fluid replacement defined by most trials as 20ml/kg bolus followed by 3ml/kg/hr compared to moderate fluid replacement which was defined differently by all trials ranging from 10ml/kg followed by 1.5ml/kg/hr. to 5-10ml/kg/hr. Dichotomous outcomes were reported as relative risk (RR) along with 95% confidence intervals (CI) while continuous outcomes were reported as mean difference (MD) along with 95% CI.
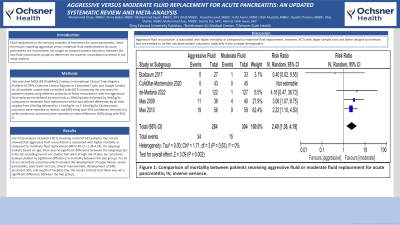
Results: Our meta-analysis included 6 RCTs involving a total of 632 patients. Our results showed that aggressive fluid resuscitation is associated with higher mortality as compared to moderate fluid replacement (RR=2.40, CI= 1.38-4.19). On subgroup analysis based on age, there was no significant difference between the subgroups (p= 0.45). On excluding two of our studies that were at high risk of bias, our sensitivity analysis yielded no significant difference in mortality between the two groups. For all of our secondary outcomes which included the development of organ failure, severe pancreatitis, pancreatic necrosis, clinical improvement, development of SIRS, persistent SIRS, and length of hospital stay, the results indicate that there was not a significant difference between the two groups.
Discussion: Aggressive fluid resuscitation is associated with higher mortality as compared to moderate fluid replacement. However, RCTs with larger sample sizes and better designs to minimize bias are needed to further elucidate patient outcomes, especially in the younger demographic.

Disclosures:
Muhammad Ehsan, MBBS1, Aamna Badar Ahmad, MBBS1, Muhammad Ayyan, MBBS1, Afra Zahid, MBBS1, Haseeba Javed, MBBS1, Hafiz Sheheryar Aamir, MBBS1, Biah Mustafa, MBBS1, Huzaifa Ahmad Cheema, MBBS1, Abia Shahid, MBBS1, Muhammad Abdullah Ilyas, MBBS1, Sophia Haroon Dar, MD2, Rehmat Ullah Awan, MD3. P1445 - Aggressive versus Moderate Fluid Replacement for Acute Pancreatitis: An Updated Systematic Review and Meta-Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1King Edward Medical University, Lahore, Punjab, Pakistan; 2Northshore-Long Island Jewish Medical Center, New York, NY; 3Ochsner Rush Medical Center, Meridian, MS
Introduction: Fluid replacement is the primary modality of treatment for acute pancreatitis. Since the results regarding aggressive versus moderate fluid replenishment for acute pancreatitis are inconsistent, we sought to compare patient outcomes between the two fluid resuscitation groups to determine the superior resuscitation protocol in our meta-analysis.
Methods: We searched MEDLINE (PubMed), Embase, International Clinical Trials Registry Platform (ICTRP), Cochrane Central Register of Controlled Trials, and Google Scholar for all available randomized controlled trials (RCTs) assessing the outcomes for patients treated using different protocols of fluids resuscitation with the aggressive fluid replacement defined by most trials as 20ml/kg bolus followed by 3ml/kg/hr compared to moderate fluid replacement which was defined differently by all trials ranging from 10ml/kg followed by 1.5ml/kg/hr. to 5-10ml/kg/hr. Dichotomous outcomes were reported as relative risk (RR) along with 95% confidence intervals (CI) while continuous outcomes were reported as mean difference (MD) along with 95% CI.
Results: Our meta-analysis included 6 RCTs involving a total of 632 patients. Our results showed that aggressive fluid resuscitation is associated with higher mortality as compared to moderate fluid replacement (RR=2.40, CI= 1.38-4.19). On subgroup analysis based on age, there was no significant difference between the subgroups (p= 0.45). On excluding two of our studies that were at high risk of bias, our sensitivity analysis yielded no significant difference in mortality between the two groups. For all of our secondary outcomes which included the development of organ failure, severe pancreatitis, pancreatic necrosis, clinical improvement, development of SIRS, persistent SIRS, and length of hospital stay, the results indicate that there was not a significant difference between the two groups.
Discussion: Aggressive fluid resuscitation is associated with higher mortality as compared to moderate fluid replacement. However, RCTs with larger sample sizes and better designs to minimize bias are needed to further elucidate patient outcomes, especially in the younger demographic.

Figure: Figure 1: Comparison of mortality between patients receiving aggressive fluid or moderate fluid replacement for acute pancreatitis; IV, inverse variance.
Disclosures:
Muhammad Ehsan indicated no relevant financial relationships.
Aamna Badar Ahmad indicated no relevant financial relationships.
Muhammad Ayyan indicated no relevant financial relationships.
Afra Zahid indicated no relevant financial relationships.
Haseeba Javed indicated no relevant financial relationships.
Hafiz Sheheryar Aamir indicated no relevant financial relationships.
Biah Mustafa indicated no relevant financial relationships.
Huzaifa Ahmad Cheema indicated no relevant financial relationships.
Abia Shahid indicated no relevant financial relationships.
Muhammad Abdullah Ilyas indicated no relevant financial relationships.
Sophia Haroon Dar indicated no relevant financial relationships.
Rehmat Ullah Awan indicated no relevant financial relationships.
Muhammad Ehsan, MBBS1, Aamna Badar Ahmad, MBBS1, Muhammad Ayyan, MBBS1, Afra Zahid, MBBS1, Haseeba Javed, MBBS1, Hafiz Sheheryar Aamir, MBBS1, Biah Mustafa, MBBS1, Huzaifa Ahmad Cheema, MBBS1, Abia Shahid, MBBS1, Muhammad Abdullah Ilyas, MBBS1, Sophia Haroon Dar, MD2, Rehmat Ullah Awan, MD3. P1445 - Aggressive versus Moderate Fluid Replacement for Acute Pancreatitis: An Updated Systematic Review and Meta-Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
