Monday Poster Session
Category: Biliary/Pancreas
P1450 - New-Onset Diabetes Mellitus and the Risk of Pancreatic Adenocarcinoma: A Propensity Matched Population-Level Study Using Hemoglobin A1c
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Oyedotun Babajide, MBBS
One Brooklyn Health
Brooklyn, NY
Presenting Author(s)
Oyedotun Babajide, MBBS1, Aakash Desai, MD2, Ayooluwatomiwa Adekunle, MD, MPH3, Michael Youssef, MD4, Mary Sedarous, MD5, Bishoy Lawendy, MD6, Philip Okafor, MD, MPH7
1One Brooklyn Health, Brooklyn, NY; 2MetroHealth Medical Center, Case Western Reserve University, Cleveland, OH; 3St. Luke’s Hospital, Chesterfield, MO; 4University of Toronto, Toronto, ON, Canada; 5Queen's University, Kingston, ON, Canada; 6University of Western Ontario, London, ON, Canada; 7Mayo Clinic Florida, Jacksonville, FL
Introduction: Seminal studies have linked diabetes mellitus (DM) with pancreatic adenocarcinoma (PDAC) mostly using fasting blood glucose levels. We sought to validate the risk of PDAC in patients with new-onset DM using hemoglobin A1c levels given the difficulty in ascertaining if glucose levels used in prior studies were truly fasting.
Methods: We performed a retrospective cohort study using data from TriNetX, a multi-institutional database of over 79 million patients across 49 healthcare organizations. Patients ≥18 years old with a diagnosis of DM determined by the ICD-10 codes and hemoglobin A1c ≥6.5 from 2006-2022 were included in the analysis cohort. Patients with a history of pancreatic neuroendocrine tumors, pancreas surgery, and/or PDAC before a diagnosis of DM were excluded. We assessed PDAC risk within 2 years of new-onset DM compared to a non-DM cohort after 1:1 propensity score matching for age, gender, race, tobacco, alcohol, chronic pancreatitis, exocrine pancreatic insufficiency, BMI, and family history of GI or pancreatic malignancy. PDAC risk was expressed as adjusted odds ratios (aOR) with 95% confidence intervals.
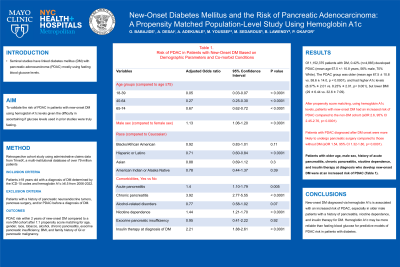
Results: Of 1,152,375 patients with DM, 0.42% (n=4,883) developed PDAC (mean age 67.5 +/- 10.8 years, 56% male, 70% White). The PDAC group was older (mean age 67.5 ± 10.8 vs. 58.6 ± 14.0, p < 0.0001), and had higher A1c levels (8.37% ± 2.01 vs. 8.23% ± 2.01, p< 0.001), but lower BMI (29 ± 6.44 vs. 32.6 ± 7.09). After propensity score matching, using hemoglobin A1c levels, patients with new-onset DM had an increased risk of PDAC compared to the non-DM cohort (aOR 2.6, 95% CI 2.45-2.76, p< 0.0001). Furthermore, patients with PDAC diagnosed after DM onset were more likely to undergo pancreatic surgery compared to those without DM (aOR 1.54, 95% CI 1.32-1.80, p< 0.0001). However, there was no difference in all-cause mortality between the DM and non-DM cohorts (aOR 0.95, 95% CI 0.89-1.007, p = 0.15). Patients with older age, male sex, history of acute pancreatitis, chronic pancreatitis, nicotine dependence, and insulin therapy at diagnosis who develop new-onset DM were at an increased risk of PDAC (Table 1).
Discussion: New-onset DM diagnosed via hemoglobin A1c is associated with an increased risk of PDAC, especially in older male patients with a history of pancreatitis, nicotine dependence, and insulin therapy for DM. Hemoglobin A1c may be more reliable than fasting blood glucose for predictive models of PDAC risk in patients with diabetes.
Disclosures:
Oyedotun Babajide, MBBS1, Aakash Desai, MD2, Ayooluwatomiwa Adekunle, MD, MPH3, Michael Youssef, MD4, Mary Sedarous, MD5, Bishoy Lawendy, MD6, Philip Okafor, MD, MPH7. P1450 - New-Onset Diabetes Mellitus and the Risk of Pancreatic Adenocarcinoma: A Propensity Matched Population-Level Study Using Hemoglobin A1c, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1One Brooklyn Health, Brooklyn, NY; 2MetroHealth Medical Center, Case Western Reserve University, Cleveland, OH; 3St. Luke’s Hospital, Chesterfield, MO; 4University of Toronto, Toronto, ON, Canada; 5Queen's University, Kingston, ON, Canada; 6University of Western Ontario, London, ON, Canada; 7Mayo Clinic Florida, Jacksonville, FL
Introduction: Seminal studies have linked diabetes mellitus (DM) with pancreatic adenocarcinoma (PDAC) mostly using fasting blood glucose levels. We sought to validate the risk of PDAC in patients with new-onset DM using hemoglobin A1c levels given the difficulty in ascertaining if glucose levels used in prior studies were truly fasting.
Methods: We performed a retrospective cohort study using data from TriNetX, a multi-institutional database of over 79 million patients across 49 healthcare organizations. Patients ≥18 years old with a diagnosis of DM determined by the ICD-10 codes and hemoglobin A1c ≥6.5 from 2006-2022 were included in the analysis cohort. Patients with a history of pancreatic neuroendocrine tumors, pancreas surgery, and/or PDAC before a diagnosis of DM were excluded. We assessed PDAC risk within 2 years of new-onset DM compared to a non-DM cohort after 1:1 propensity score matching for age, gender, race, tobacco, alcohol, chronic pancreatitis, exocrine pancreatic insufficiency, BMI, and family history of GI or pancreatic malignancy. PDAC risk was expressed as adjusted odds ratios (aOR) with 95% confidence intervals.
Results: Of 1,152,375 patients with DM, 0.42% (n=4,883) developed PDAC (mean age 67.5 +/- 10.8 years, 56% male, 70% White). The PDAC group was older (mean age 67.5 ± 10.8 vs. 58.6 ± 14.0, p < 0.0001), and had higher A1c levels (8.37% ± 2.01 vs. 8.23% ± 2.01, p< 0.001), but lower BMI (29 ± 6.44 vs. 32.6 ± 7.09). After propensity score matching, using hemoglobin A1c levels, patients with new-onset DM had an increased risk of PDAC compared to the non-DM cohort (aOR 2.6, 95% CI 2.45-2.76, p< 0.0001). Furthermore, patients with PDAC diagnosed after DM onset were more likely to undergo pancreatic surgery compared to those without DM (aOR 1.54, 95% CI 1.32-1.80, p< 0.0001). However, there was no difference in all-cause mortality between the DM and non-DM cohorts (aOR 0.95, 95% CI 0.89-1.007, p = 0.15). Patients with older age, male sex, history of acute pancreatitis, chronic pancreatitis, nicotine dependence, and insulin therapy at diagnosis who develop new-onset DM were at an increased risk of PDAC (Table 1).
Discussion: New-onset DM diagnosed via hemoglobin A1c is associated with an increased risk of PDAC, especially in older male patients with a history of pancreatitis, nicotine dependence, and insulin therapy for DM. Hemoglobin A1c may be more reliable than fasting blood glucose for predictive models of PDAC risk in patients with diabetes.
Disclosures:
Oyedotun Babajide indicated no relevant financial relationships.
Aakash Desai indicated no relevant financial relationships.
Ayooluwatomiwa Adekunle indicated no relevant financial relationships.
Michael Youssef indicated no relevant financial relationships.
Mary Sedarous indicated no relevant financial relationships.
Bishoy Lawendy indicated no relevant financial relationships.
Philip Okafor indicated no relevant financial relationships.
Oyedotun Babajide, MBBS1, Aakash Desai, MD2, Ayooluwatomiwa Adekunle, MD, MPH3, Michael Youssef, MD4, Mary Sedarous, MD5, Bishoy Lawendy, MD6, Philip Okafor, MD, MPH7. P1450 - New-Onset Diabetes Mellitus and the Risk of Pancreatic Adenocarcinoma: A Propensity Matched Population-Level Study Using Hemoglobin A1c, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
