Monday Poster Session
Category: Biliary/Pancreas
P1452 - ERCP in Liver Transplant Recipients: A Nationwide Analysis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Khaled Elfert, MD
SBH Health System
Bronx, NY
Presenting Author(s)
Khaled Elfert, MD1, Azizullah Beran, MD2, Mohamed Ahmed, MD3, Islam Mohamed, MD4, Khalid K. Ahmed, MD5, Tamta Chkhikvadze, MD6, Ahmad Al-Taee, MD7, Suresh Nayudu, MD1
1SBH Health System, Bronx, NY; 2Indiana University, Indianapolis, IN; 3University of Missouri Kansas City, Overland Park, KS; 4University of Missouri-Kansas City, Kansas City, MO; 5The Wright Center for GME, Scranton, PA; 6SUNY Downstate Health Sciences University, Brooklyn, NY; 7University of Illinois at Urbana–Champaign, Champaign, IL
Introduction: Biliary complications, including biliary strictures, leakage, and obstruction due to stones or sludge, are common after liver transplant. ERCP is a crucial procedure for managing these complications. Our study aims to assess ERCP outcomes in patients with liver transplant and to investigate the common indications for ERCP in those patients utilizing a nationwide representative sample.
Methods: We conducted an analysis of the National Inpatient Sample database from 2016 to 2020, that included patients who underwent ERCP (Endoscopic Retrograde Cholangiopancreatography). Patients younger than 18 years old were excluded from the study. The patient population was divided into two categories based on liver transplant status, and we compared baseline characteristics and clinical outcomes between the two groups using chi-square tests and Student's t-tests.
Results: Our analysis included a total of 1,070,310 hospitalizations in the non-liver transplant group and 5,800 patients in the liver transplant group. The mean age was 60 years in the non-liver transplant group and 57 years in the liver transplant group. There were more male patients in the transplant group, and a higher percentage of patients had a Charleston comorbidity index of 3 or above in the transplant group (Table 1).
To investigate the common indications of ERCP in liver transplant recipients, we examined this cohort's most common principal diagnoses. The principal diagnosis was bile duct obstruction in 13.36%, post-surgical and liver transplant-related complications in 13.01%, cholangitis in 9.74%, and sepsis in 8.62% of the hospitalizations.
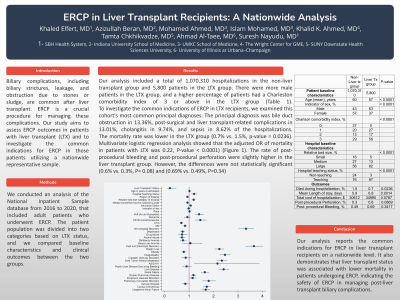
The mortality rate was lower in the liver transplant group (0.7% vs. 1.5%, p-value = 0.0236). Multivariate logistic regression analysis showed that the adjusted OR of mortality in patients with liver transplant was 0.22, P-value < 0.0001) (Figure 1). The rate of post-procedural bleeding and post-procedural perforation were slightly higher in the liver transplant group. However, the differences were not statistically significant (0.6% vs. 0.3%, P= 0.08) and (0.69% vs. 0.49%, P=0.34)
Discussion: Our analysis reports the common indications for ERCP in liver transplant recipients on a nationwide level. It also demonstrates that liver transplant status was associated with lower mortality in patients undergoing ERCP, indicating the safety of ERCP in managing post-liver transplant biliary complications.

Disclosures:
Khaled Elfert, MD1, Azizullah Beran, MD2, Mohamed Ahmed, MD3, Islam Mohamed, MD4, Khalid K. Ahmed, MD5, Tamta Chkhikvadze, MD6, Ahmad Al-Taee, MD7, Suresh Nayudu, MD1. P1452 - ERCP in Liver Transplant Recipients: A Nationwide Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1SBH Health System, Bronx, NY; 2Indiana University, Indianapolis, IN; 3University of Missouri Kansas City, Overland Park, KS; 4University of Missouri-Kansas City, Kansas City, MO; 5The Wright Center for GME, Scranton, PA; 6SUNY Downstate Health Sciences University, Brooklyn, NY; 7University of Illinois at Urbana–Champaign, Champaign, IL
Introduction: Biliary complications, including biliary strictures, leakage, and obstruction due to stones or sludge, are common after liver transplant. ERCP is a crucial procedure for managing these complications. Our study aims to assess ERCP outcomes in patients with liver transplant and to investigate the common indications for ERCP in those patients utilizing a nationwide representative sample.
Methods: We conducted an analysis of the National Inpatient Sample database from 2016 to 2020, that included patients who underwent ERCP (Endoscopic Retrograde Cholangiopancreatography). Patients younger than 18 years old were excluded from the study. The patient population was divided into two categories based on liver transplant status, and we compared baseline characteristics and clinical outcomes between the two groups using chi-square tests and Student's t-tests.
Results: Our analysis included a total of 1,070,310 hospitalizations in the non-liver transplant group and 5,800 patients in the liver transplant group. The mean age was 60 years in the non-liver transplant group and 57 years in the liver transplant group. There were more male patients in the transplant group, and a higher percentage of patients had a Charleston comorbidity index of 3 or above in the transplant group (Table 1).
To investigate the common indications of ERCP in liver transplant recipients, we examined this cohort's most common principal diagnoses. The principal diagnosis was bile duct obstruction in 13.36%, post-surgical and liver transplant-related complications in 13.01%, cholangitis in 9.74%, and sepsis in 8.62% of the hospitalizations.
The mortality rate was lower in the liver transplant group (0.7% vs. 1.5%, p-value = 0.0236). Multivariate logistic regression analysis showed that the adjusted OR of mortality in patients with liver transplant was 0.22, P-value < 0.0001) (Figure 1). The rate of post-procedural bleeding and post-procedural perforation were slightly higher in the liver transplant group. However, the differences were not statistically significant (0.6% vs. 0.3%, P= 0.08) and (0.69% vs. 0.49%, P=0.34)
Discussion: Our analysis reports the common indications for ERCP in liver transplant recipients on a nationwide level. It also demonstrates that liver transplant status was associated with lower mortality in patients undergoing ERCP, indicating the safety of ERCP in managing post-liver transplant biliary complications.

Figure: Figure 1 demonstrates the forest plot for the multivariate logistic regression analysis for mortality in patients undergoing ERCP.
Disclosures:
Khaled Elfert indicated no relevant financial relationships.
Azizullah Beran indicated no relevant financial relationships.
Mohamed Ahmed indicated no relevant financial relationships.
Islam Mohamed indicated no relevant financial relationships.
Khalid Ahmed indicated no relevant financial relationships.
Tamta Chkhikvadze indicated no relevant financial relationships.
Ahmad Al-Taee indicated no relevant financial relationships.
Suresh Nayudu indicated no relevant financial relationships.
Khaled Elfert, MD1, Azizullah Beran, MD2, Mohamed Ahmed, MD3, Islam Mohamed, MD4, Khalid K. Ahmed, MD5, Tamta Chkhikvadze, MD6, Ahmad Al-Taee, MD7, Suresh Nayudu, MD1. P1452 - ERCP in Liver Transplant Recipients: A Nationwide Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
