Monday Poster Session
Category: Biliary/Pancreas
P1454 - Comparative Meta-Analysis of Endoscopic Ultrasound-Guided Cholecystoduodenostomy and Cholecystogastrostomy in the Treatment of Gallbladder Disease: Symptom Resolution and Complication Rates
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Clive J. Miranda, DO, MS
University at Buffalo
Buffalo, NY
Presenting Author(s)
Clive J. Miranda, DO, MS1, Hassam Ali, MD2, Sourabh Goyal, DO1, Alexander M. Carlson, DO1, Rashmi R. Advani, MD3
1University at Buffalo, Buffalo, NY; 2East Carolina University, Greenville, NC; 3Cedars-Sinai Medical Center, Los Angeles, CA
Introduction: Cholecystectomy is the treatment of choice for most patients with acute cholecystitis. Malignancies or advanced comorbidities, however, can preclude surgical intervention but patients can still achieve gallbladder drainage either percutaneously or endoscopically. Endoscopic ultrasound (EUS)-guided transmural gallbladder drainage has recently gained favor, establishing a conduit from the gallbladder to the stomach (cholecystogastrostomy, EUS-CG) or duodenum (cholecystoduodenostomy, EUS-CD) via various stent or catheter types. Literature on the safety and efficacy of these techniques is currently limited to scattered cases and cohort studies. Here, we provide a meta-analysis on symptom resolution and complication rates between the two techniques.
Methods: A comprehensive search of PubMed, OVID, CINAHL, and Cochrane databases was conducted to identify literature on EUS-CG or EUS-CD usage between 2012-2022. 6 studies were analyzed describing both techniques. The risk ratio was calculated utilizing a random-effects model (Mantel-Haenszel method, 95% Confidence Interval) with the assistance of Revman 5.4 and GPT-4 (Wolfram API). The heterogeneity of the studies was assessed and reported through I2.
Results: A total of 69 patients (34 male, 35 female, mean age 72 years) undergoing endoscopic gallbladder drainage for various types of gallbladder disease were identified. EUS-CG was performed in 24 patients and EUS-CD in 45. The most common procedural indication was acute cholecystitis, with symptomatic cholelithiasis and malignant biliary obstruction as the next most common indications. All patients had preprocedural symptoms with varying degrees of abdominal pain, vomiting, fever, and jaundice. The most common procedural complications were fever (9%) and abdominal pain (5%). Two patients died from post-procedural aspiration pneumonia and pancreatic infection. Both techniques demonstrated comparable symptom resolution with an overall risk ratio of 1.04 (95% CI: 0.85-1.29), and no significant difference was found (Z = 0.41, P = 0.68). Additionally, both techniques showed similar complication rates with an overall risk ratio of 0.84 (95% CI: 0.42-1.70), and no significant difference was observed (Z = 0.47, P = 0.64).
Discussion: Both EUS-CG and EUS-CD demonstrate similar rates of symptom resolution and complication rates in nonsurgical candidates requiring gallbladder drainage. Further studies with larger patient cohorts are needed to better understand the efficacy between these two techniques.

Disclosures:
Clive J. Miranda, DO, MS1, Hassam Ali, MD2, Sourabh Goyal, DO1, Alexander M. Carlson, DO1, Rashmi R. Advani, MD3. P1454 - Comparative Meta-Analysis of Endoscopic Ultrasound-Guided Cholecystoduodenostomy and Cholecystogastrostomy in the Treatment of Gallbladder Disease: Symptom Resolution and Complication Rates, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University at Buffalo, Buffalo, NY; 2East Carolina University, Greenville, NC; 3Cedars-Sinai Medical Center, Los Angeles, CA
Introduction: Cholecystectomy is the treatment of choice for most patients with acute cholecystitis. Malignancies or advanced comorbidities, however, can preclude surgical intervention but patients can still achieve gallbladder drainage either percutaneously or endoscopically. Endoscopic ultrasound (EUS)-guided transmural gallbladder drainage has recently gained favor, establishing a conduit from the gallbladder to the stomach (cholecystogastrostomy, EUS-CG) or duodenum (cholecystoduodenostomy, EUS-CD) via various stent or catheter types. Literature on the safety and efficacy of these techniques is currently limited to scattered cases and cohort studies. Here, we provide a meta-analysis on symptom resolution and complication rates between the two techniques.
Methods: A comprehensive search of PubMed, OVID, CINAHL, and Cochrane databases was conducted to identify literature on EUS-CG or EUS-CD usage between 2012-2022. 6 studies were analyzed describing both techniques. The risk ratio was calculated utilizing a random-effects model (Mantel-Haenszel method, 95% Confidence Interval) with the assistance of Revman 5.4 and GPT-4 (Wolfram API). The heterogeneity of the studies was assessed and reported through I2.
Results: A total of 69 patients (34 male, 35 female, mean age 72 years) undergoing endoscopic gallbladder drainage for various types of gallbladder disease were identified. EUS-CG was performed in 24 patients and EUS-CD in 45. The most common procedural indication was acute cholecystitis, with symptomatic cholelithiasis and malignant biliary obstruction as the next most common indications. All patients had preprocedural symptoms with varying degrees of abdominal pain, vomiting, fever, and jaundice. The most common procedural complications were fever (9%) and abdominal pain (5%). Two patients died from post-procedural aspiration pneumonia and pancreatic infection. Both techniques demonstrated comparable symptom resolution with an overall risk ratio of 1.04 (95% CI: 0.85-1.29), and no significant difference was found (Z = 0.41, P = 0.68). Additionally, both techniques showed similar complication rates with an overall risk ratio of 0.84 (95% CI: 0.42-1.70), and no significant difference was observed (Z = 0.47, P = 0.64).
Discussion: Both EUS-CG and EUS-CD demonstrate similar rates of symptom resolution and complication rates in nonsurgical candidates requiring gallbladder drainage. Further studies with larger patient cohorts are needed to better understand the efficacy between these two techniques.

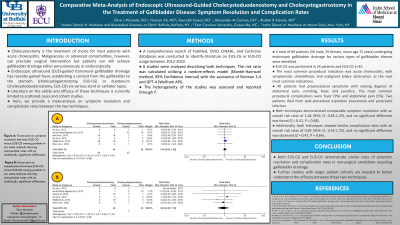
Figure: Figure A: Forest plot on symptom resolution between EUS-CG versus EUS-CD among patients in our meta-analysis showing comparable rates with no statistically significant difference.
Figure B: Forest plot on complications between EUS-CG versus EUS-CD among patients in our meta-analysis showing comparable rates with no statistically significant difference.
Figure B: Forest plot on complications between EUS-CG versus EUS-CD among patients in our meta-analysis showing comparable rates with no statistically significant difference.
Disclosures:
Clive Miranda indicated no relevant financial relationships.
Hassam Ali indicated no relevant financial relationships.
Sourabh Goyal indicated no relevant financial relationships.
Alexander Carlson indicated no relevant financial relationships.
Rashmi Advani indicated no relevant financial relationships.
Clive J. Miranda, DO, MS1, Hassam Ali, MD2, Sourabh Goyal, DO1, Alexander M. Carlson, DO1, Rashmi R. Advani, MD3. P1454 - Comparative Meta-Analysis of Endoscopic Ultrasound-Guided Cholecystoduodenostomy and Cholecystogastrostomy in the Treatment of Gallbladder Disease: Symptom Resolution and Complication Rates, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
