Monday Poster Session
Category: Biliary/Pancreas
P1456 - Progression from Recurrent Acute to Chronic Pancreatitis During Long-Term Follow-Up of Up to 22 Years in a Well-Defined North American Cohort
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Vu Dinh, MD, PhD
University of Pittsburgh Medical Center
Cranberry Township, PA
Presenting Author(s)
Award: Presidential Poster Award
Vu Dinh, MD, PhD1, Ravy Vajravelu, MD, MSCE2, Chaeryon Kang, PhD2, Melissa Saul, MS2, Anna Phillips, MD, MS3, Randall Brand, MD3, Adam Slivka, MD, PhD3, David Whitcomb, MD, PhD3, Dhiraj Yadav, MD, MPH3
1University of Pittsburgh Medical Center, Cranberry Township, PA; 2University of Pittsburgh, Pittsburgh, PA; 3University of Pittsburgh Medical Center, Pittsburgh, PA
Introduction: According to the mechanistic definition, in the disease continuum from acute (AP) to chronic pancreatitis (CP), patients who experience recurrent acute pancreatitis (RAP) are a high-risk group. An accurate assessment of risk and factors associated with progression can inform primary and secondary prevention strategies for CP. We hypothesized that demographic, patient and disease-related factors affect the risk of incident CP.
Methods: We reviewed data for 195 RAP patients enrolled in the North American Pancreatitis Studies (NAPS2) from UPMC between 2000-2014 who had follow-up information available. Baseline data were retrieved from NAPS2 database while follow-up information was collected by review of electronic health records. The primary outcome of interest was a new diagnosis of CP (defined by any combination of pancreatic calcifications, moderate-severe pancreatic duct dilatation, stricture and/or atrophy). Censoring criteria included the date at first occurrence of either - diagnosis of CP, death, date of last contact or end of follow-up period (10/2022). We used multivariable Cox regression models with stepwise selection procedure to evaluate the impact of covariates of interest (demographics, patient and disease-related factors) on incident CP during follow-up.
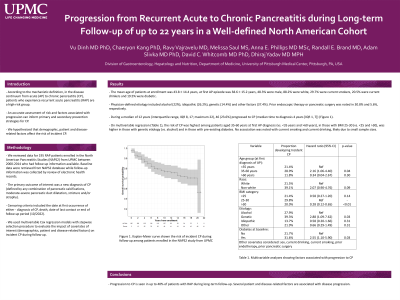
Results: The mean age of patients at enrollment was 43.8±14.4 years, at first AP episode was 38.6±15.2 years, 48.3% were male, 88.2% were white, 29.7% were current smokers, 20.5% were current drinkers and 19.5% were diabetic. Physician-defined etiology included alcohol (22%), idiopathic (26.2%), genetic (14.4%) and other factors (37.4%). Prior endoscopic therapy or pancreatic surgery was noted in 30.8% and 5.6%, respectively. During a median of 12 years (interquartile range, IQR 8, 17; maximum 22), 46 (23.6%) progressed to CP (median time to diagnosis 4 years [IQR 1, 7]) (Figure 1). On multivariable regression (Table 1), the risk of CP was highest among patients aged 35-60 years at first AP diagnosis (vs. < 35 years and >60 years), in those with BMI 25-30 (vs. < 25 and >30), was higher in those with genetic etiology (vs. alcohol) and in those with pre-existing diabetes. No association was noted with current smoking and current drinking likely due to small sample sizes.
Discussion: Progression to CP is seen in up to 40% of patients with RAP during long-term follow-up. Several patient and disease-related factors are associated with disease progression.

Disclosures:
Vu Dinh, MD, PhD1, Ravy Vajravelu, MD, MSCE2, Chaeryon Kang, PhD2, Melissa Saul, MS2, Anna Phillips, MD, MS3, Randall Brand, MD3, Adam Slivka, MD, PhD3, David Whitcomb, MD, PhD3, Dhiraj Yadav, MD, MPH3. P1456 - Progression from Recurrent Acute to Chronic Pancreatitis During Long-Term Follow-Up of Up to 22 Years in a Well-Defined North American Cohort, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Vu Dinh, MD, PhD1, Ravy Vajravelu, MD, MSCE2, Chaeryon Kang, PhD2, Melissa Saul, MS2, Anna Phillips, MD, MS3, Randall Brand, MD3, Adam Slivka, MD, PhD3, David Whitcomb, MD, PhD3, Dhiraj Yadav, MD, MPH3
1University of Pittsburgh Medical Center, Cranberry Township, PA; 2University of Pittsburgh, Pittsburgh, PA; 3University of Pittsburgh Medical Center, Pittsburgh, PA
Introduction: According to the mechanistic definition, in the disease continuum from acute (AP) to chronic pancreatitis (CP), patients who experience recurrent acute pancreatitis (RAP) are a high-risk group. An accurate assessment of risk and factors associated with progression can inform primary and secondary prevention strategies for CP. We hypothesized that demographic, patient and disease-related factors affect the risk of incident CP.
Methods: We reviewed data for 195 RAP patients enrolled in the North American Pancreatitis Studies (NAPS2) from UPMC between 2000-2014 who had follow-up information available. Baseline data were retrieved from NAPS2 database while follow-up information was collected by review of electronic health records. The primary outcome of interest was a new diagnosis of CP (defined by any combination of pancreatic calcifications, moderate-severe pancreatic duct dilatation, stricture and/or atrophy). Censoring criteria included the date at first occurrence of either - diagnosis of CP, death, date of last contact or end of follow-up period (10/2022). We used multivariable Cox regression models with stepwise selection procedure to evaluate the impact of covariates of interest (demographics, patient and disease-related factors) on incident CP during follow-up.
Results: The mean age of patients at enrollment was 43.8±14.4 years, at first AP episode was 38.6±15.2 years, 48.3% were male, 88.2% were white, 29.7% were current smokers, 20.5% were current drinkers and 19.5% were diabetic. Physician-defined etiology included alcohol (22%), idiopathic (26.2%), genetic (14.4%) and other factors (37.4%). Prior endoscopic therapy or pancreatic surgery was noted in 30.8% and 5.6%, respectively. During a median of 12 years (interquartile range, IQR 8, 17; maximum 22), 46 (23.6%) progressed to CP (median time to diagnosis 4 years [IQR 1, 7]) (Figure 1). On multivariable regression (Table 1), the risk of CP was highest among patients aged 35-60 years at first AP diagnosis (vs. < 35 years and >60 years), in those with BMI 25-30 (vs. < 25 and >30), was higher in those with genetic etiology (vs. alcohol) and in those with pre-existing diabetes. No association was noted with current smoking and current drinking likely due to small sample sizes.
Discussion: Progression to CP is seen in up to 40% of patients with RAP during long-term follow-up. Several patient and disease-related factors are associated with disease progression.

Figure: Figure 1. Kaplan-Meier curve showing the risk of incident CP during follow-up among patients enrolled in the NAPS2 study from UPMC
Disclosures:
Vu Dinh indicated no relevant financial relationships.
Ravy Vajravelu indicated no relevant financial relationships.
Chaeryon Kang indicated no relevant financial relationships.
Melissa Saul indicated no relevant financial relationships.
Anna Phillips indicated no relevant financial relationships.
Randall Brand indicated no relevant financial relationships.
Adam Slivka indicated no relevant financial relationships.
David Whitcomb indicated no relevant financial relationships.
Dhiraj Yadav indicated no relevant financial relationships.
Vu Dinh, MD, PhD1, Ravy Vajravelu, MD, MSCE2, Chaeryon Kang, PhD2, Melissa Saul, MS2, Anna Phillips, MD, MS3, Randall Brand, MD3, Adam Slivka, MD, PhD3, David Whitcomb, MD, PhD3, Dhiraj Yadav, MD, MPH3. P1456 - Progression from Recurrent Acute to Chronic Pancreatitis During Long-Term Follow-Up of Up to 22 Years in a Well-Defined North American Cohort, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

