Monday Poster Session
Category: Biliary/Pancreas
P1465 - GlycA: A New Biomarker of Disease Activity and Severity in Acute Pancreatitis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
- IS
Ishani Shah, MD
University of Utah School of Medicine
Salt Lake City, Utah
Presenting Author(s)
Ishani Shah, MD1, William Yakah, PhD2, Awais Ahmed, MD3, Steven Freedman, MD, PhD3, Zhenghui jiang, MD, PhD4, Margery A. Connelly, PhD, MBA5, Sunil G. Sheth, MD3
1University of Utah School of Medicine, Salt Lake City, UT; 2Columbia University, New York, NY; 3Beth Israel Deaconess Medical Center, Boston, MA; 4Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA; 5Labcorp, Morrisville, NC
Introduction: Acute pancreatitis (AP) is a leading cause of gastrointestinal hospital admissions with up to 40% mortality in moderate-severe AP. Glycoprotein acetylation (GlycA) is measured as a nuclear magnetic resonance signal (NMR) of post-translational modification of glycosylated acute phase proteins released during inflammation. We aimed to investigate the role of GlycA as an inflammatory biomarker of AP.
Methods: We prospectively enrolled AP patients (n=20) and healthy controls (n=22) and collected EDTA plasma samples at admission and discharge. NMR spectra were acquired from these samples using a 400 MHz Vantera® Clinical Analyzer and GlycA concentrations were calculated (normal = 400 mmol/L). The GlycA NMR signal, at 2.00 ± 0.01 ppm in the NMR spectrum, is derived from the N-acetyl methyl group protons within the carbohydrate side chains of circulating glycoproteins such as α1-acid glycoprotein, haptoglobin, α1-antitrypsin, α1-antichymotrypsin and transferrin. GlycA levels were then compared between AP patients and controls as well as within the AP group based on etiology and severity.
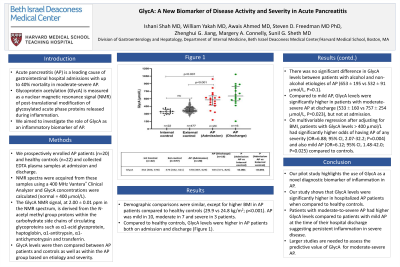
Results: Demographic comparisons were similar, except for higher BMI in AP patients compared to healthy controls (29.9 vs 24.8 kg/m2; p< 0.001). AP was mild in 10, moderate in 7 and severe in 3 patients. Compared to healthy controls, GlycA levels were higher in AP patients both on admission and discharge (Figure 1). There was no significant difference in GlycA levels between patients with alcohol and non-alcohol etiologies of AP (653 ± 195 vs 532 ± 91 mmol/L, P=0.1). Compared to mild AP, GlycA levels were significantly higher in patients with moderate-severe AP at discharge (533 ± 160 vs 757 ± 254 mmol/L, P=0.023), but not at admission. On multivariable regression after adjusting for BMI, patients with GlycA levels > 400 mmol/L had significantly higher odds of having AP of any severity (OR=6.88; 95% CI, 2.07-32.2; P=0.004) and also mild AP (OR=6.12; 95% CI, 1.48-42.0; P=0.025) compared to controls.
Discussion: Our pilot study highlights the use of GlycA as a novel diagnostic biomarker of inflammation in AP. Our study shows that GlycA levels were significantly higher in hospitalized AP patients when compared to healthy controls. Patients with moderate-to-severe AP had higher GlycA levels compared to patients with mild AP at the time of their hospital discharge suggesting persistent inflammation in severe disease. Larger studies are needed to assess the predictive value of GlycA for moderate-severe AP.

Disclosures:
Ishani Shah, MD1, William Yakah, PhD2, Awais Ahmed, MD3, Steven Freedman, MD, PhD3, Zhenghui jiang, MD, PhD4, Margery A. Connelly, PhD, MBA5, Sunil G. Sheth, MD3. P1465 - GlycA: A New Biomarker of Disease Activity and Severity in Acute Pancreatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Utah School of Medicine, Salt Lake City, UT; 2Columbia University, New York, NY; 3Beth Israel Deaconess Medical Center, Boston, MA; 4Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA; 5Labcorp, Morrisville, NC
Introduction: Acute pancreatitis (AP) is a leading cause of gastrointestinal hospital admissions with up to 40% mortality in moderate-severe AP. Glycoprotein acetylation (GlycA) is measured as a nuclear magnetic resonance signal (NMR) of post-translational modification of glycosylated acute phase proteins released during inflammation. We aimed to investigate the role of GlycA as an inflammatory biomarker of AP.
Methods: We prospectively enrolled AP patients (n=20) and healthy controls (n=22) and collected EDTA plasma samples at admission and discharge. NMR spectra were acquired from these samples using a 400 MHz Vantera® Clinical Analyzer and GlycA concentrations were calculated (normal = 400 mmol/L). The GlycA NMR signal, at 2.00 ± 0.01 ppm in the NMR spectrum, is derived from the N-acetyl methyl group protons within the carbohydrate side chains of circulating glycoproteins such as α1-acid glycoprotein, haptoglobin, α1-antitrypsin, α1-antichymotrypsin and transferrin. GlycA levels were then compared between AP patients and controls as well as within the AP group based on etiology and severity.
Results: Demographic comparisons were similar, except for higher BMI in AP patients compared to healthy controls (29.9 vs 24.8 kg/m2; p< 0.001). AP was mild in 10, moderate in 7 and severe in 3 patients. Compared to healthy controls, GlycA levels were higher in AP patients both on admission and discharge (Figure 1). There was no significant difference in GlycA levels between patients with alcohol and non-alcohol etiologies of AP (653 ± 195 vs 532 ± 91 mmol/L, P=0.1). Compared to mild AP, GlycA levels were significantly higher in patients with moderate-severe AP at discharge (533 ± 160 vs 757 ± 254 mmol/L, P=0.023), but not at admission. On multivariable regression after adjusting for BMI, patients with GlycA levels > 400 mmol/L had significantly higher odds of having AP of any severity (OR=6.88; 95% CI, 2.07-32.2; P=0.004) and also mild AP (OR=6.12; 95% CI, 1.48-42.0; P=0.025) compared to controls.
Discussion: Our pilot study highlights the use of GlycA as a novel diagnostic biomarker of inflammation in AP. Our study shows that GlycA levels were significantly higher in hospitalized AP patients when compared to healthy controls. Patients with moderate-to-severe AP had higher GlycA levels compared to patients with mild AP at the time of their hospital discharge suggesting persistent inflammation in severe disease. Larger studies are needed to assess the predictive value of GlycA for moderate-severe AP.

Figure: Figure 1: GlycA levels in healthy control subjects compared to patients with AP during hospitalization
Disclosures:
Ishani Shah indicated no relevant financial relationships.
William Yakah indicated no relevant financial relationships.
Awais Ahmed indicated no relevant financial relationships.
Steven Freedman indicated no relevant financial relationships.
Zhenghui jiang indicated no relevant financial relationships.
Margery Connelly indicated no relevant financial relationships.
Sunil G. Sheth indicated no relevant financial relationships.
Ishani Shah, MD1, William Yakah, PhD2, Awais Ahmed, MD3, Steven Freedman, MD, PhD3, Zhenghui jiang, MD, PhD4, Margery A. Connelly, PhD, MBA5, Sunil G. Sheth, MD3. P1465 - GlycA: A New Biomarker of Disease Activity and Severity in Acute Pancreatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
