Monday Poster Session
Category: Biliary/Pancreas
P1467 - A New Approach to Evaluating the Microbiome of the Pancreas
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Megan B. Ghai, MD, MPH, MA
University of Arizona College of Medicine
Phoenix, AZ
Presenting Author(s)
Megan B. Ghai, MD, MPH, MA1, Jianing Yang, MD, PhD1, Jose Aponte-Pieras, MD2, Jennifer Li, BS1, Mahmoud Bayoumi, MD, MPH3, Melisa P. Celaya, PhD4, Frederic Zenhausern, PhD1, Wahid Wassef, MD, MPH, FACG5
1University of Arizona College of Medicine, Phoenix, AZ; 2Kirk Kerkorian School of Medicine at UNLV, Las Vegas, NV; 3University of Tennessee, Knoxville, TN; 4University of Arizona, Phoenix, AZ; 5Banner University Medical Center, Phoenix, AZ
Introduction: Chronic pancreatitis (CP) is an inflammatory-mediated condition with irreversible morphological changes leading to pancreatic endocrine and exocrine dysfunction. Disruptions in the microbial balance can be associated with many inflammatory-mediated pathologies including CP. The analysis of the microbiome in pancreatic disease has largely relied on using fecal or salivary samples. Few studies have directly analyzed duodenal fluid aspirate of pancreatic exocrine secretions. In this pilot study, we aimed to prove feasibility of using duodenal fluid aspirate and molecular profiling to characterize the pancreatic microbiome.
Methods: Included were adults who had already been referred for an endoscopic ultrasound (EUS) with secretin testing for work up of suspected CP. Those excluded were exposed to antibiotics within 30 days of EUS, undergoing chemotherapy, or had a history of Roux-en-y gastric bypass. Secretin was administered pre-procedurally. Using EUS, duodenal fluid was aspirated at time t= 0, 15-, 30-, 45-, and 60-minutes post-secretin administration. Microbial analysis was performed on isolated DNA with the IS-pro Microbiota kit and software. The microbial analyses were correlated to the secretin study results to identify participants with CP.
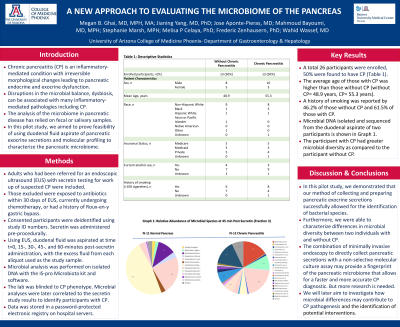
Results: A total of 28 participants were enrolled, 53.6% were found to have CP. Descriptive statistics are presented in Table 1. Of note, the average age of those with CP was higher than those without CP (without CP= 48.9 years, CP= 53.7 years). A history of smoking was reported by 46.2% of those without CP and 60% of those with CP. Microbial DNA isolated and sequenced from the duodenal aspirate of two participants is shown in Graph 1. The participant with CP had greater microbial diversity as compared to the participant without CP.
Discussion: In this pilot study, we demonstrated that our method of collecting and preparing pancreatic exocrine secretions successfully allowed for the identification of bacterial species. We were also able to characterize differences in microbial diversity between those with and without CP. The combination of minimally invasive endoscopy to directly collect pancreatic secretions with a non-selective molecular culture assay may provide a fingerprint of the pancreatic microbiome that allows for a faster and more accurate CP diagnostic. We will later aim to investigate how microbial differences may contribute to CP pathogenesis and the identification of potential interventions.

Disclosures:
Megan B. Ghai, MD, MPH, MA1, Jianing Yang, MD, PhD1, Jose Aponte-Pieras, MD2, Jennifer Li, BS1, Mahmoud Bayoumi, MD, MPH3, Melisa P. Celaya, PhD4, Frederic Zenhausern, PhD1, Wahid Wassef, MD, MPH, FACG5. P1467 - A New Approach to Evaluating the Microbiome of the Pancreas, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Arizona College of Medicine, Phoenix, AZ; 2Kirk Kerkorian School of Medicine at UNLV, Las Vegas, NV; 3University of Tennessee, Knoxville, TN; 4University of Arizona, Phoenix, AZ; 5Banner University Medical Center, Phoenix, AZ
Introduction: Chronic pancreatitis (CP) is an inflammatory-mediated condition with irreversible morphological changes leading to pancreatic endocrine and exocrine dysfunction. Disruptions in the microbial balance can be associated with many inflammatory-mediated pathologies including CP. The analysis of the microbiome in pancreatic disease has largely relied on using fecal or salivary samples. Few studies have directly analyzed duodenal fluid aspirate of pancreatic exocrine secretions. In this pilot study, we aimed to prove feasibility of using duodenal fluid aspirate and molecular profiling to characterize the pancreatic microbiome.
Methods: Included were adults who had already been referred for an endoscopic ultrasound (EUS) with secretin testing for work up of suspected CP. Those excluded were exposed to antibiotics within 30 days of EUS, undergoing chemotherapy, or had a history of Roux-en-y gastric bypass. Secretin was administered pre-procedurally. Using EUS, duodenal fluid was aspirated at time t= 0, 15-, 30-, 45-, and 60-minutes post-secretin administration. Microbial analysis was performed on isolated DNA with the IS-pro Microbiota kit and software. The microbial analyses were correlated to the secretin study results to identify participants with CP.
Results: A total of 28 participants were enrolled, 53.6% were found to have CP. Descriptive statistics are presented in Table 1. Of note, the average age of those with CP was higher than those without CP (without CP= 48.9 years, CP= 53.7 years). A history of smoking was reported by 46.2% of those without CP and 60% of those with CP. Microbial DNA isolated and sequenced from the duodenal aspirate of two participants is shown in Graph 1. The participant with CP had greater microbial diversity as compared to the participant without CP.
Discussion: In this pilot study, we demonstrated that our method of collecting and preparing pancreatic exocrine secretions successfully allowed for the identification of bacterial species. We were also able to characterize differences in microbial diversity between those with and without CP. The combination of minimally invasive endoscopy to directly collect pancreatic secretions with a non-selective molecular culture assay may provide a fingerprint of the pancreatic microbiome that allows for a faster and more accurate CP diagnostic. We will later aim to investigate how microbial differences may contribute to CP pathogenesis and the identification of potential interventions.

Figure: Graph 1. Relative Abundance of Microbial Species at 45 minutes Post Secretin Administration. Microbial diversity between a patient with and without chronic pancreatitis are compared. The patient with chronic pancreatitis has relatively increased microbial diversity.
Disclosures:
Megan Ghai indicated no relevant financial relationships.
Jianing Yang indicated no relevant financial relationships.
Jose Aponte-Pieras indicated no relevant financial relationships.
Jennifer Li indicated no relevant financial relationships.
Mahmoud Bayoumi indicated no relevant financial relationships.
Melisa Celaya indicated no relevant financial relationships.
Frederic Zenhausern indicated no relevant financial relationships.
Wahid Wassef indicated no relevant financial relationships.
Megan B. Ghai, MD, MPH, MA1, Jianing Yang, MD, PhD1, Jose Aponte-Pieras, MD2, Jennifer Li, BS1, Mahmoud Bayoumi, MD, MPH3, Melisa P. Celaya, PhD4, Frederic Zenhausern, PhD1, Wahid Wassef, MD, MPH, FACG5. P1467 - A New Approach to Evaluating the Microbiome of the Pancreas, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
